NHS 75: A family affair

Working in Poole Hospital, and born in Poole Hospital to parents who met at Poole Hospital, we speak to Ellen Sinden about her NHS story….
I started working in Poole in 1998 when I completed my pre-registration year as a pharmacist with Boots. The pharmacy was next to the old main entrance and you used to stand at the long wooden bench, dispensing and checking prescriptions while gazing out on to Longfleet Road. There was always a lot of excitement when the fire engine arrived, likely to an occasion of burnt toast!
In those days you wore white lab coats and used light counters to count out tablets from large dispensing pots. There was a dumbwaiter like lift system that bought drugs up from he pharmacy stores and jars of leeches and packs of maggots to treat things like skin ulcers.
Now the lab coats have been replaced with dark scrub tops, the light counters have been taken over by pre-packed packs of tablets and dispensing robots now store and deliver the tablets to the dispensing bench. And no leeches
….but this is not when it started for my family. Thirty years earlier, in 1968, Nurse Rumens (my mum aged 18) and Nurse Sinden (my dad aged 22) were just starting their nurse training at Poole Hospital. They were enrolled in the two-year ‘state enrolled nursing’ (SEN) course, rotating round different areas under the watchful eye of the sister.

Ellen's parents: Nurse Rumens, far left, and Nurse Sinden, centre
Mum’s accommodation was in ‘tampax towers’ as it was fondly called and there was a firm midnight curfew. There was a strict uniform policy - stiff, starch cleaned clothes – and your appearance was regularly inspected by the sister and matron.
My mum’s rotation into outpatients was bought to a halt when my dad (who had bad asthma at the time and wasn’t allowed into theatres) was transferred into her slot. This disappointment couldn’t have lasted long as shortly after this they were married! After the wedding, mum visited her patients in her wedding dress and gave out wedding cake.
Dad started working on A2 which was a trauma ward dealing mainly with road traffic accidents. He moved into Coronary Care (CCU) and was there until he passed away in October 1998. People have fond memories of my dad smoking his pipe while walking up the corridor!
…. back to the present day and I am still working at Poole Hospital, now as a practitioner within rheumatology. Changes are always happening within the NHS, and aren’t easy, but we should be extremely proud of the NHS’ achievements. After all, it’s where my parents met and is why I’m here today!

Ellen Sinden, practitioner in rheumatology
Planning for the future
Today the NHS published the first ever NHS Long Term Workforce Plan – a plan developed by the NHS, backed by investment from government and created in collaboration with our staff and experts.
This will deliver the biggest increase in training numbers in our 75-year history with record numbers of nurses, doctors, dentists, Allied Health Professionals and other key healthcare staff to address the gaps in the current workforce and meet the challenge of a growing and ageing population.
Since the founding of the NHS 75 years ago, we have relied on the skill and dedication of staff who came here from around the world, and there will always be a place for them in the NHS. But as global demand for healthcare workers grows, we need to train more people here to future proof the NHS.
Increasing recruitment is not enough on its own so we are also setting out how we will retain more staff and use tech to free up them up to do what they do best: care for patients.
Our staff have told us that they want opportunities to progress and learn throughout their working life, so this plan also looks at how to deliver on the commitments in the NHS People Promise, ensuring we can attract and retain talent and support our teams.
Things will not change overnight but this NHS workforce plan represents a once in a generation opportunity to put staffing on a sustainable footing.
Read the full plan at www.england.nhs.uk/LongTermWorkforcePlan
Milestone bell boosts morale for patients with cancer
A patient undergoing cancer treatment at the Royal Bournemouth Hospital (RBH) has donated a symbolic bell for his fellow patients to ring when a they reach a treatment milestone.
David Le Monnier, from Jersey has been in treatment since January and has been a regular patient at RBH. Currently on his fourth round of chemotherapy and waiting for a bone marrow transplant, he was inspired to donate the bell when seeing other patients on the ward.
David explained: “I recently went home for 10 days rest from treatment. When I came back into the department, I saw another patient being applauded by staff as she left after her final treatment.
“She asked if there was a bell, she could ring but the team said unfortunately there wasn’t. This was my lightbulb moment!
“This bell is for any and all patients. I want anyone who achieves anything to ring the bell. Although it is for patients in their treatment, I also want staff to ring it if they have had a good day at work. All achievements are important.”
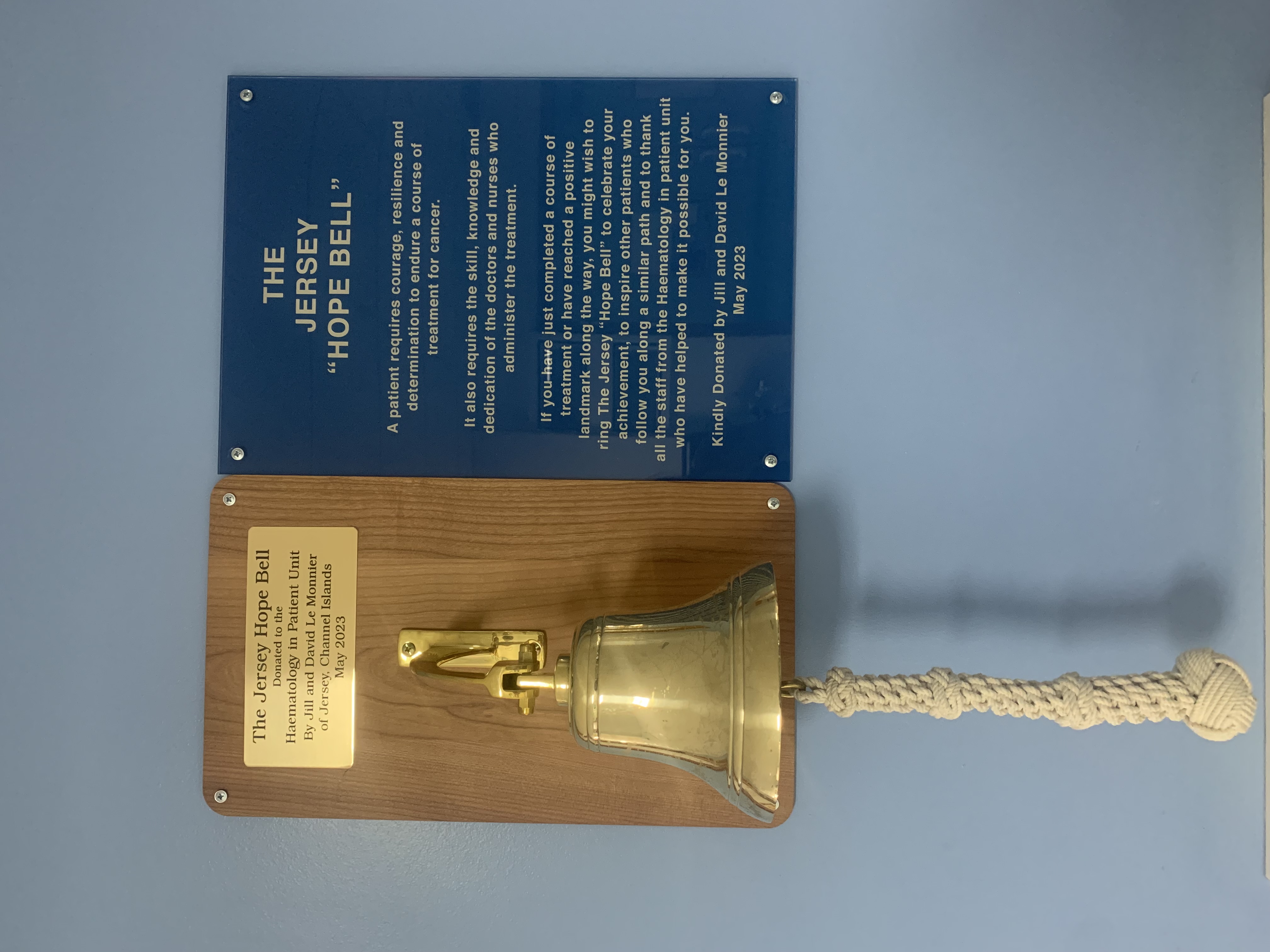
The bell has been named the ‘Jersey Hope Bell’ and sits alongside this special message to fellow patients and those looking after them:
“A patient requires courage, resilience and determination to endure a course of treatment for cancer. It also requires the skill, knowledge and dedication of the doctors and nurses who administer the treatment.
“If you have just completed a course of treatment or have reached a positive landmark along the way, you might wish to ring the ‘Jersey Hope Bell’ to celebrate your achievement, to inspire other patients who follow you along a similar path and to thank all the staff from haematology in patient unit who have helped make it possible for you”.
Marie Miller, senior matron for cancer care, said: “As a team we really appreciate receiving the bell from David. Having a bell to celebrate the success milestones of a patients receiving their treatment is a massive boost not only for patients, but their families and our team. It is great that we can all come together to recognise this.”
David added: “I had the opportunity to ring the bell as I left for my break in treatment. It is very loud – it probably woke the whole ward up!”

Funding boost to strengthen hospital links with Africa
A University Hospitals Dorset (UHD) consultant has secured £65,000 in funding to support an educational programme in Uganda around better use of antibiotics.
Dr Pasco Hearn, consultant microbiologist, applied for the funding after a trip to Lira in Uganda last year. The trip was part of the Poole Africa Link programme, which sees teams from the hospital visit the local university and hospital in Lira to provide training.

The £65,000 funding, from the Tropical Health Education Trust and the Commonwealth Pharmacists' Association, will be used to bolster the microbiology labs in Lira Hospital and to encourage clinicians there to re-look at how they use antibiotics. Medics from Lira will also visit UHD to share their experiences.

The focus will be on ‘teaching the teacher’, establishing infection prevention and antimicrobial champions who will continue the work for the benefit of the community for years to come.
Millions of pounds is spent on antibiotics every year by the NHS and antibiotic resistance is one of the biggest threats to global health, food security, and development today.
Dr Hearn said: “Antibiotic resistance can affect anyone, of any age, in any country and can lead to longer hospital stays, higher medical costs and increased deaths. However, we can do something to reduce the impact and limit the spread of resistance.”
“Visiting Uganda, you see first-hand the constraints of working within limited resources, something we are often asked to do now in the NHS. It is also a healthy reminder that the world is not a fair place and that the NHS is a valuable and extraordinary service that we are lucky to have,” he added.
The Poole Africa Link trips are an opportunity for UHD staff to hone their skills at making pragmatic decisions, help spread the positives of a no-blame culture, learn how to plan and deliver succinct education, and importantly, support individual wellbeing.
Dr Hearn said: “It can be a challenging environment to work in but we are no strangers to challenges working in the NHS. As we mark our NHS’ 75th birthday, it feels only right that we take the core values of ‘improving lives’ and ‘commitment to quality of care’ to a global community.”
You can find out more about Poole Africa Link at pooleafricalink.org.uk
Well Women’s Event for people with Learning Disabilities held by Dorset Breast Screening Unit.
Dorset Breast Screening Unit (DBSU) held their first Well Women’s Event for people with learning disabilities to be introduced to our cancer screening and other women's health services.
DBSU invited women and their carers from across Dorset to come and learn more about the benefits of screening and to see for themselves what is involved to help make them more relaxed at any future appointments.
Victoria Cannings from Dorset Cancer Partnership said: “Today’s event was focussed on helping to reduce heath inequalities – we want everyone to use our screening services and to feel comfortable when they do. We hope by showing people what is involved and answering any questions they or their carers may have before their screening that they will book and keep appointments and when they do come to us, they will be prepared.”
Teams from breast, bowel and cervical screening were all on hand to answer questions and we also had a menopause team there too as often symptoms are missed or not understood. Teams from Dorset MIND, Live Well Dorset, Cancer Matters Wessex, and People First Forum also attended. Twenty people joined us on the open day and we had two women booked in for their screening following the event."
Chelsey Pope, Interim Breast Manager from UHD, added: “The open day just before Learning Disability Week went very well and we were glad to have the opportunity to speak to women about any concerns they may have regarding their breast screening. We had some easy-read leaflets that explained more about screening and attendees were given the opportunity to walk around the unit and see the x-ray and ultrasound rooms and ask questions of staff on how they work. Since the event we have had very positive feedback, including one lady saying she would no longer be frightened to attend the unit, which was what we hoped to achieve.”
The open day was organised in conjunction with Dorset Cancer Partnership and supported by Dorset Mind, Live Well Dorset, Cancer Matters Wessex, People First Forum, and NHS Dorset. Future open days are now being planned, including one focussed for men.










