Postnatal care
Mothers/birthing people and babies who have had a more complicated birth experience and who have not been able to go home directly from the Haven Unit or Woodland Labour Ward, will remain on the Mulberry postnatal ward until they are fit to go home. We are here to help you to get fit and ready to go home as soon as possible.
Within 72 hours of birth your baby will have a full neonatal examination by a neonatologist or appropriately trained midwife either whilst you are in hospital, in the postnatal clinic or at home.
What to bring in
Each room on the Mulberry postnatal ward has a small bedside locker with room for a change of clothes and toiletries. A cot is provided for your baby. This has cupboard space for baby clothing and changing items.
You will need:
For you
- Any medication you are taking
- Comfortable clothing – loose t-shirts with room for baby to be tucked in and held in skin-to-skin contact
- Dressing gown
- Slippers
- Night wear
- Nursing bra and breast pads
- Ordinary or disposable pants
- Two packs of maternity-size sanitary towels
- Toiletries
- Bath towel
For your baby
- Nappies
- Vest and babygro
- If you have made an informed decision to formula feed, you will need to bring in a starter pack of ready made infant formula milk (stage one or first milk).
- Cotton wool
Please do not bring in a car seat for your baby until you are ready to go home.
Infant feeding
The maternity unit at Bournemouth is committed to encouraging mums to feed their baby via their chosen method, and we would like you to be successful with this.
If you have made an informed decision to bottle feed your baby, you will be given the appropriate care and support, but the hospital does not provide formula milk, unless your baby requires it for medical reasons. In all other cases you will be expected to provide formula milk yourself. If you choose to bottle feed, please ensure that you bring in your own supplies of ready-made infant formula milk for the newborn (starter pack). On average, your baby will require 6-8 feeds per 24 hour period so please ensure that you bring in sufficient supplies.
Visiting times on the Mulberry postnatal ward are as follows:
- We suggest that visitors attend during the core hours of: 10am-8pm (this includes children of the mother/birthing person and their partner)
- One support partner can stay on site at all times
We do not allow children who are not baby’s brother or sister to visit.
- The Breastfeeding Network - lists all current local groups via postcode and you can follow them on Facebook and Instagram here.
- Building a Happy Baby - A Guide for Parents
- https://maternitymattersdorset.nhs.uk/after/feeding/
- Start for Life Feeding Information
- https://www.unicef.org.uk/babyfriendly/
- http://www.unicef.org.uk/BabyFriendly/Resources/Resources-for-parents/Department-of-Health-bottle-feeding-leaflet/
- Breastfeeding Support in the Community
- Breastfeeding Support Groups in Dorset
Respecting our staff and patients
The trust operates a zero tolerance policy on abuse towards staff or patients. If you are asked to leave, please do so.
Patient information
Please click on the links below to download information leaflets:
Caring for your wound after a caesarean section
Advice on third and fourth degree perineal tears during childbirth
Advice of third and fourth degree tears - advice for opening your bowels
Pain relief in labour
There are many different methods which can be used to help relieve pain during labour.
There are some fantastic benefits of using a birthing pool in labour. Even if you do not wish to have a waterbirth, water can be a wonderful form of pain relief as it is calming and relaxing. Water pools are available in the Maternity Unit at the Royal Bournemouth Hospital.
Other benefits include:
- A greater feeling of control and choice
- It can shorten the length of your labour
- Less painful contractions
- Less likely to need an epidural for pain relief
- Relaxing and contributes towards a feeling of wellbeing
- Aids buoyancy and offers support to allow you to change position more easily, encouraging your baby to get in the best position possible for the birth
- Reduces anxiety, muscle spasm and tension
Transcutaneous Electrical Nerve Stimulation (TENS)
A TENS machine is a small battery-operated pulsar which sends gentle electrical impulses through four electrodes taped to your back. The machine is designed for use in labour, and the impulses stimulate your body to produce natural pain-relieving hormones called endorphins which will help your body cope with the contractions. TENS is most effective if used from early labour, as it takes around 30 to 40 minutes to build up the endorphin levels and the electrical stimulation can be increased as the contractions become more intense.
Your birth partner or companion can apply the TENS at home while in early labour and you may use it for the journey to hospital and then throughout your labour. Using TENS gives you the freedom to move around and change your position.
It is not possible to use the TENS in water, so if you wish to use the birthing pool you should remove the TENS. However, water works in a very similar manner by encouraging your body to increase its natural endorphins. If you leave the pool the TENS can be reconnected with very little loss of effect.
There are no known side-effects, but TENS should not be used if you have epilepsy or a pacemaker. Do not use your TENS machine before 37 weeks of pregnancy.
Paracetamol
Paracetamol may be taken by mouth in tablet or solution form. It is particularly useful in early labour at home. It can help during early labour, allowing you to have some rest, but will become less effective as your labour progresses.
Although rare, some women may experience side effects as listed on the packaging. Paracetamol should not be taken if it is known that you have an intolerance or allergy to it.
Entonox ('gas and air')
Entonox is a gas which is a mixture of 50% oxygen and 50% nitrous oxide. Many women refer to it as ‘gas and air’. The gas is piped from a wall attachment or can come from a cylinder. The gas is breathed in through a mouthpiece during a contraction to reduce the intensity of the contractions. To get the best effect, the timing is very important – your midwife will help you with this. Each mouthpiece is disposable and only used for one woman. Entonox is available in the Maternity Unit at the Royal Bournemouth Hospital and via your community midwife if you are having a home birth.
If you choose to use Entonox you will hold the tube yourself, which enables you to control how much you have. The effects of Entonox wear off very quickly once you stop using it, usually within a few minutes. Entonox can be used with other pain relief and can be used in the birthing pool. It can also be used at any time during labour and in any position.
Pethidine
Pethidine is a strong pain-killing injection, from a group of drugs known as opioids. An opioid injection is normally given into your buttock or leg. You can have two injections during your labour, four hours apart. You can have pethidine if you are having your baby at home too.
After a pethidine injection you will probably feel very sleepy and relaxed, and you may even go to sleep in between your contractions. You may feel sick after you have the injection, but we can give you something to reduce this effect at the same time.
Because it is likely that you will become drowsy, you may be less mobile, but your midwife will advise you on adopting active birth positions in which you will still be able to rest.
Remifentanil
Remifentanil is a strong morphine-like painkiller that works very quickly and wears off equally quickly. Although it cannot provide total pain relief it has been shown to significantly reduce pain from contractions.
What is patient controlled analgesia (PCA)?
Remifentanil is given in small doses through a tube placed in one of your veins. The PCA machine contains the remifentanil which is connected to this tube. You will be given a button to hold that, when you press it, will make the PCA pump give you a small amount of remifentanil. The PCA has a timer on it so you cannot give yourself too much of the drug.
Who can use it?
Remifentanil is mainly reserved for women who cannot have an epidural. However, if you decide to try the remifentanil and do not like it you can still decide to have an epidural instead if there is no other reason for you not to have one. It is not safe to use if you have an allergy or sensitivity to morphine-like drugs, or your anaesthetist or obstetrician advise against it.
How do I use it?
The pain relieving effects happen within 20-30 seconds of pressing the button. You should press the button as soon as you feel a contraction starting. The effects will wear off in minutes. You can continue to use it up until your baby is born.
Are there any side effects?
Some women do find that the remifentanil has some side effects. These include feeling sleepy, sick or dizzy. You may also feel itchy. However these will rapidly disappear once the drug is stopped. Some women find it slows their breathing and occasionally the amount of oxygen in their blood falls. This is easily treated by giving you oxygen but because of this you will need to have a small clip on your finger while you are using the PCA to monitor your blood oxygen levels. Remifentanil does cross the placenta to the baby in a similar way to pethidine but, unlike pethidine, any effect wears off much more quickly. This type of pain relief has now been used in large numbers of women in labour with no side effects to the baby.
When can I ask for the PCA?
You can have the PCA at any time once your midwife has confirmed you are in active labour and your anaesthetist has agreed that it is safe for you to use.
Epidural
The nerves from your womb and surrounding muscles pass through the lower part of your spine to reach the brain. Most of the pain felt during labour comes from these nerves. An epidural is an anaesthetic which is injected into this part of your spine to numb the nerves so you don't feel the contractions as much during labour.
An anaesthetist performs the procedure. A drip is inserted into a vein in your hand or arm. Your back is cleaned and local anaesthetic is injected. Then, a fine hollow tube (known as a catheter) is inserted into your back whilst you sit up very still, curled forwards. This is securely taped into place so that you can freely move into comfortable positions on the bed. Pain relieving drugs are then given through this catheter continually by a pump. The epidural aims to provide adequate, sometimes complete, pain relief within about 20 minutes. If the pain relief is complete, you will be able to rest.
Are there any side effects?
Normally epidural analgesia (pain relief) is straightforward and very effective, with little risk of harmful effects. Some complications of pregnancy and some blood disorders may make epidural unsuitable for you – your midwife and doctor will advise you about this.
Epidurals may cause low blood pressure, and for this reason you will be given a drip in your arm so that we can give you fluids to try to prevent low blood pressure. Your baby’s heartbeat will also be monitored continuously when you have an epidural in place.
Approximately 1 in 100 women can experience a headache after an epidural. If this happens it can be treated, but it is unpleasant.
You will have reduced sensation to your bottom, hips and legs and may lose feeling altogether. Normal sensation will return within a few hours after you have had your baby.
Types of birth
There are a number of ways to give birth. Some women need more support than others. and this information is intended to give an overview of the different types of birth available
Vaginal birth
A vaginal birth takes place naturally, without help from the doctors. The midwife looks after you and helps you to achieve a vaginal birth. You can have a vaginal birth at home or in hospital, whether you have a long or short labour, and when you have had a previous birth which was not vaginal. A vaginal birth can also be achieved using a birthing pool.
After your baby is born the midwife will help you with the delivery of the afterbirth (placenta). This is usually straightforward and takes just a few minutes, and there are two options for the delivery of the placenta. Many women choose to have an injection to help the placenta separate; this is known as ‘active management’ and the midwife will ask for your consent before administering this. The other option is known as ‘physiological management’, where you do not have an injection, and the placenta is delivered naturally. This usually takes longer, and your midwife will advise you on how this is done.
What sort of pain relief can I have for vaginal birth?
You can have whatever choice of pain relief you would like. Please see our ‘Pain Relief in Labour’ tab for all pain relief options offered in the maternity service.
Will I need to have stitches?
Sometimes a tear occurs at the point of birth, which will need stitches to help it to heal.There are ways to reduce the severity of your tear. Please discuss these with your community midwife. These will be put in by your midwife or a doctor shortly after your baby’s birth. Sometimes there is no tear at all, or a small tear occurs which does not need any stitches. Your midwife will advise you. Occasionally with a vaginal birth it may be necessary to perform a surgical cut (episiotomy) if your baby is unwell and needs to be delivered quickly, or you are showing signs of an extensive tear.
For some women, a vaginal birth will not be possible, but this is something which you, your partner and your midwife can discuss together. Our main priority is ensuring mothers and babies are well.
Vacuum extraction (Ventouse/suction)
Vacuum extraction may be performed when mother or baby is too tired during labour, but the reasons will always be explained to you.
The extractor consists of a cap provided by a small machine that a doctor attaches to your baby’s head. The baby is then gently guided through the birth canal whilst you push during contractions. Once your baby’s head is born, the cap is removed and your baby’s body is born.
Forceps delivery
Forceps are metal instruments like large spoons. A doctor places the forceps around the baby’s head to cradle it. Your baby is then guided through the birth canal as you push with your contractions. Once your baby’s head is born, the forceps are removed, and your baby’s body is born. There are three types of forceps used (named after the people who invented them), and the reasons they are used are explained below:
- Wrigley’s (low forceps) – these are simple forceps used when your baby’s head is facing the right direction, and is low down in the birth canal
- Anderson’s (straight forceps) – these are used if your baby is not as far down in the birth canal
- Kielland’s (rotational forceps) – these are used if your baby’s head needs help to turn slightly before they are guided down the birth canal
Forceps deliveries are always performed by a doctor.
What sort of pain relief can I have for a vacuum or a forceps?
If you have already got an Epidural for pain relief, this can easily be topped up for either a vacuum or a forceps birth. If you have used other types of pain relief or ways of coping with contractions, the doctor is likely to use what is known as a ‘Pudendal block’. This is a local anaesthetic (pain relief) in the form of an injection, which blocks the pain around your vagina. Sometimes it is recommended that you have a spinal anaesthetic for forceps, but your midwife, doctor, or anaesthetist will advise you about this. A spinal anaesthetic is similar to an Epidural, but has very quick action.
Will I need to have an episiotomy?
An episiotomy is a cut made into the tissues at the back of the vagina and is sometimes used for a vacuum or forceps birth. It is not always possible to tell whether it is necessary until the time of birth, but the doctor and midwife will speak to you about it. If it is necessary, the doctor will make sure that you are numb at the area before the episiotomy is carried out, and that the stitches are put in straight away.
Will I need stitches?
Sometimes a vacuum birth can be carried out without the need for stitches afterwards, but often a tear occurs which may need stitches.
It is more likely that you will need stitches following a forceps birth. However, the doctor will put the stitches in very quickly after your baby is born, and together with the midwife, they will make sure that you have some pain relief. Your midwife at home or on the ward afterwards will advise you on caring for your stitches, and keeping comfortable.
Benefits of ventouse/forceps birth
- The birth will be aided when there is a need
- Your baby will be born more quickly if there is a concern for either you or your baby, or if you are very tired
Risks or disadvantages
- Some women feel a lot of discomfort following this type of birth; your midwife will advise you on managing this
- Some women feel disappointed that they have not achieved a ‘vaginal’ birth: your midwife will provide support for you
- Sometimes the ventouse cap or the forceps will leave a mark on your baby’s head – this mark will fade over 48 hours
Caesarean section
There are many reasons why a caesarean section, or C-section, is performed, but mainly it is recommended when there is a medical indication that a vaginal birth may not be safe either for you or your baby. There are a number of situations where you and your doctor or midwife may feel that the risks of vaginal delivery are increased and outweigh those of caesarean section; such indications can be identified before labour (e.g. if the placenta covers the neck of the womb (cervix) or if the womb has been weakened by previous surgery) or during labour e.g if the fetal heart rate monitoring suggests that the fetus is not getting enough oxygen.
In these cases, where it is clearly safer for you and the baby to be delivered by C-section, the doctor/midwife will discuss the risks with you and arrange for a caesarean section with your consent.
A C-section is a surgical operation where your baby is born through a cut in the abdominal wall. The cut is usually along the top of the pubic hairline, so the scar can be well hidden when healed. It is always performed by a doctor in an operating theatre, and a midwife will be with you at all times.
A caesarean section is sometimes performed as an emergency operation when you are in labour. When this happens, many things will be going on at the same time, but your midwife will always be with you. The doctors and midwife will ensure that you understand the reasons for the surgery and will ask for your consent before carrying out the operation.
If you have already had an epidural for pain relief, it is very likely that this will be topped up for your operation. Otherwise the anaesthetist will put in a spinal (which is very similar to an epidural, but works very quickly). Very rarely, you may need to have a general anaesthetic and be asleep for your operation. When you go into the theatre for your operation, there will be many different noises, people who you have not yet met, and very bright lights. However you will always have your midwife with you, your birth partner can come with you, and all the members of staff in the theatre are there to help you have your baby safely. Once your baby is born you can usually see and hold them straight away.
What if there are no medical indications and I ask for a caesarean section ?
There is a large body of evidence to support the widely-held view that pregnancy ending in vaginal delivery is a process which is safe and appropriate for women with a low predicted risk of complication in the UK.
If there are no identifiable factors that increase the risk of vaginal delivery then caesarean section will not be offered routinely as a birthing option. You might still think that a caesarean section remains the best choice for you and your baby, particularly if you have had a previous negative birthing experience, have complications during the pregnancy, or are worried about delivering vaginally.
If this is the case then you will be referred to a senior doctor or midwife with extensive experience of caesarean section and vaginal delivery. You will have the opportunity to discuss your anxieties about vaginal delivery and they will provide you with information about the relative risks and benefits of both methods of delivery. In addition, you might find it helpful to have regular meetings with a healthcare professional trained to provide psychological support during pregnancy and childbirth. Ultimately we wish to make sure that your delivery is as safe as possible for you and your baby and that you have a positive birthing experience.
What are the risks of caesarean section?
Risks for you:
- Higher risk of uterine (womb) infection
- Higher risk of severe bleeding (hemorrhage)
- Higher risk of developing a blood clot in your legs or lungs
- Risk of accidental surgical damage to your bladder or bowel
- Longer stay in hospital
Risks for baby:
- Higher risk of your baby developing breathing problems following birth requiring hospital admission
- Problems breastfeeding
Risks for future pregnancies:
- Higher chance of developing low lying placenta (placenta praevia)
- Higher chance of developing a placenta (accreta) which grows abnormally into the uterine wall and sometimes beyond; these are rare complications but are serious enough to endanger your life and that of your baby
- More chance of infertility following first caesarean section
- More chance of stillbirth
It is important to emphasize that for many of these risks, the increase related to caesarean section is small and most women having a cesarean section will not be affected by them.
Your midwife will help plan your birth with you and offer you:
- Small group birth preparation classes
- Infant feeding workshops
- Choice of the place of birth: hospital or home.
- Choice of birth companions present at the birth
- Choice of pain relief
- Water birth
- Support to feed your baby
- Support with caring for the baby after birth
Care in labour
Mums-to-be under the care of University Hospitals Dorset may choose to have their baby at home, or give birth in hospital, depending on their clinical needs:
At home
If you are fit and well, have no medical conditions and have a straightforward pregnancy, you could choose to have your baby at home.
Please click here for further details.
If you would like to discuss having a home birth in more detail please speak to your community midwife. Alternatively please ring 01202 442692, leave a message and a midwife will contact you to discuss your choice.
Haven Birthing Suite
The Haven Unit Birth Centre is our low-risk, midwife-led birthing suite. It is set in a homely environment and the emphasis is on low-intervention childbirth, and how we can empower you to achieve this.
Mothers and birthing people who are fit and well, have no medical conditions, and have a straightforward pregnancy can choose to give birth in the Haven.
The Haven has six en-suite birth rooms. The environment in the Haven is relaxed and women and birthing people are encouraged to be as active and mobile as possible in labour. Water is a fantastic method of pain relief and there are five birthing pools in the Haven for mothers and birthing people to use, either for pain relief or to birth in as well.
It is a good idea to tell us you would like to use the pool when you phone the Maternity Advice Line (MAL) on 0300 369 0388. The pools can take 10-15 minutes to fill, so we can get it ready while you are on your way in.
Low risk aids such as birthing balls and mats are freely available on the Haven. In addition, special equipment is available to help mothers and birthing people adopt comfortable positions while in labour.
Maternity Advice Line: 0300 369 0388
- Option 1 – clinical advice (24/7 cover)
- Option 2 – clerical queries (8am-4pm cover)
Woodland Labour Ward
Mothers and birthing people who have had a high risk pregnancy in the past, have an existing medical condition, have developed a complication in this pregnancy or who wish to use epidural as a method of pain relief are encouraged to give birth in the Woodland Labour Ward.
There are two birthing pools available to women/birthing people on Woodland Labour Ward, you should discuss your desire to use water for labour/birth with your midwife or obstetrician as part of your plan for birth.
It is a good idea to tell us you would like to use the pool when you phone the Maternity Advice Line (MAL) on 0300 369 0388. The pools can take 10-15 minutes to fill, so we can get it ready while you are on your way in.
When you are admitted you will be given your own room which you will normally stay in to give birth. Sometimes however it might be necessary to transfer you to the theatre for delivery, for example if you need a forceps or caesarean delivery. A midwife will be assigned to look after you. Midwives normally work 12 hour shifts. Depending on the time of your admission and the length of your labour you may have more than one midwife looking after you throughout your labour.
The rooms on Woodland Labour Ward do have quite a lot of equipment but this is there to ensure the safety of you and your baby. Most mothers/birthing people and babies in this suite need to be monitored more closely throughout labour. However we encourage mothers and birthing people to be as active as possible to increase the chances of achieving a normal birth. Continuous monitoring using telemetry is also available on the Woodland Labour Ward.
Telemetry is a remote system that permits wireless monitoring of fetal and maternal wellbeing in water or whilst moving around. This is appropriate for mothers and birthing people who need continuous monitoring and who wish to be as mobile as possible.
Other birthing aids such as balls and mats are also available on the Woodland Labour Ward, please ask your midwife if you would like to use these for labour.
Within the theatre there are two dedicated obstetric theatres for women and birthing people who require a caesarean section. These are run by a dedicated team of theatre staff. If you need to give birth in the obstetric theatre you will be accompanied by a midwife who will support you and your birth partner through the caesarean section.
For more information, please click here
Maternity Advice Line: 0300 369 0388
- Option 1 – clinical advice (24/7 cover)
- Option 2 – clerical queries (8am-4pm cover)
Baby's Movements
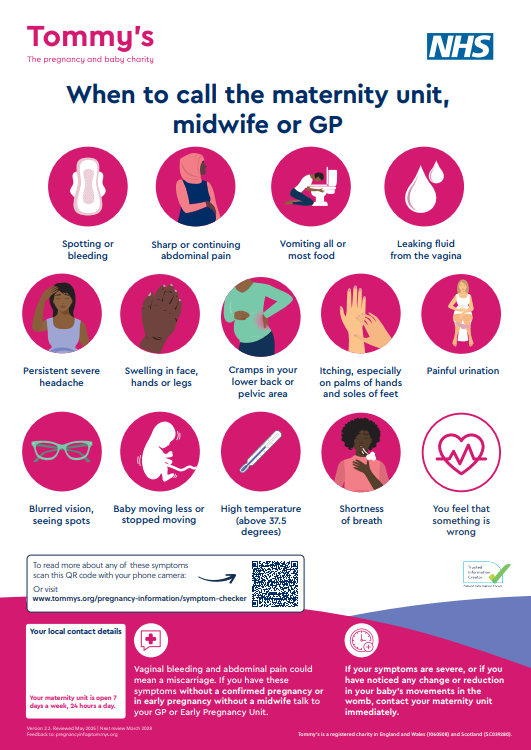
Feeling your baby move is a sign they are well. If you notice your baby’s movements have changed call Labourline 0300 369 0388.
The links below provide useful information regarding your baby's movements:
Movements matter - raising awareness of fetal movements
https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_57.pdf