Exercise and Recovery
As a result of critical illness your muscles can become very weak. Your body takes what it needs to survive from its stores in your muscles, meaning they may be smaller and weaker. It takes time to get your strength back.
Returning to normal life can seem very far away. Everyday activities such as getting out of bed, getting dressed, walking, and climbing stairs may be challenging. This section has been developed to try and aid your recovery after intensive care treatment.
Whilst you are on the ward and then at home it is important that you try and do as much as you can yourself. Staff members, carers and family will often try and help you by doing things for you. As part of your recovery, it is IMPORTANT you do as much as you can yourself safely as part of your recovery and rehabilitation such as: making yourself a drink and sitting in a chair.
Some of the benefits of exercises are:
- To maintain muscle strength.
- To maintain bone density.
- To maintain joint range of movement.
- To help improve cardiovascular fitness.
- To aid return to function and daily life.
- To maintain and improve exercise tolerance.
- To aid the recovery of the respiratory system.
- To provide positive psychological benefits.
- Help reduce stress
Tips for exercise:
Start with a low number of repetitions for each exercise (5 is often a good level). As an exercise becomes easier, gradually increase the number you do. This will build up your strength and fitness.
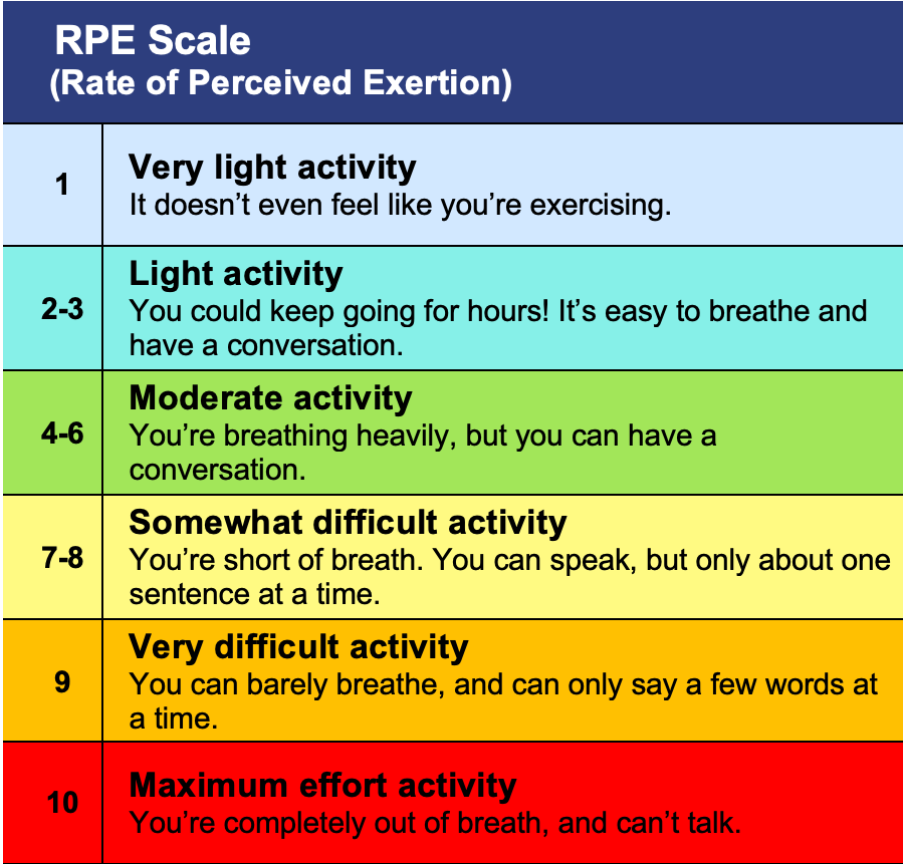
When you do exercises at home try it out and rate them using the Borg RPE exertion scale (see table below)
When performing an exercise, you want to be working between 4-6.
If when you first try an exercise, you score your exertion above 7, then this exercise is too difficult for you and you should either:
- Do fewer repetitions
- Do it for a shorter time
- Choose an easier exercise to replace it.
If on the other hand when you first do an exercise you score below 4, then this is too easy for you and you need to either:
- Increase the number of repetitions
- Increase the time you do it for
- Choose a harder exercise
- Add some weight i.e., hold a small bottle of water.
When you have completed your exercises do not forget to record them in your exercise diary and record your Borg RPE score.
Borg RPE score.
Try to do the exercises at least once a day. This can be increased to 2 – 3 times a day if you feel able or as advised by your ward therapist.
Stop exercising and rest if you experience any:
- Severe chest pain
- Increase in chest tightness
- Dizziness or feeling faint
- Severe breathlessness
Consult a doctor if these symptoms persist.
Critical Care Follow Up Service
The role of the Critical Care Follow Up Team, comprised of critical care nurses and therapists, is to support you and your relatives when you are discharged to the ward and when you are at home.
We know that patients often cannot remember their stay in critical care, where possible a patient diary is kept. If you received a diary and you have any remaining questions about your stay, please speak with the Critical Care Follow-up Team.
We will invite you back to the Critical Care follow-up clinic if you have had a prolonged stay with us. The clinic offers you an opportunity to discuss your critical care stay and any concerns or worries you may have about your recovery.
An appointment is offered 2-3 months after you have been discharged home. If you have not received a follow up appointment and would like one, or you or your family have further questions, please contact the Follow-up Team.
General Recovery
Doing a little bit more each week applies not only to exercise. Setting yourself realistic targets to achieve over the next few weeks is the way to proceed from here. If you normally enjoyed, for example, gardening or baking before your illness but have not had the energy to do this since your illness, set getting back to this as one of your targets. Start small and work up from there.
Therapy Equipment
Motomed

This is a leg & arm trainer that regulates your muscle tone or boosting circulation. It can be used in laying and seated positions.
Stryker Chair

You may not be at the stage to get into a chair by yourself. With this you are stretchered across safely and gently raised into a sitting position. Sitting out daily helps keep your chest clear and strengthen your sitting muscles.
Sara Stedy

Can support early mobility by encouraging you to be active during sitting to standing transfers e.g., from bed to chair, increasing your confidence. A seat can be put behind you, so you do not have to stand during the transfer.
ReTurn

Can be used to support early mobility for patients who are able to maintain a stand for a short period of time. It can be used to rebuild strength in core areas and assist in getting you active again. Once standing you can be wheeled short distances.
Planning recovery - Going Home
Whilst on critical care, staff involved in your recovery and rehabilitation are likely to have included Physiotherapists, Occupational Therapists, Speech and Language Therapists as well as the nurses and Doctors. They will have worked with you to improve your strength and mobility and set agreed goals for recovery.
When you are transferred to the ward your rehabilitation will continue with the therapy team responsible for that ward speciality.
The planning to get you out of hospital will start as soon as possible, with more emphasis when you are on the ward. So, when you feel able to, start thinking about where you might go when you are discharged. For example, home or to a family member or friend’s house. As you progress in your recovery you will be included in discussions about the appropriate time to be discharged home. If, at that time you still have rehabilitation goals to work towards, you will be supported with any equipment required at home and have a referral to be followed up with community therapy teams. In some circumstances it may be more appropriate for you to continue your rehabilitation at a community therapy hospital to then facilitate your discharge home.
Examples of support may include:
- Equipment in the bathroom such as a raised toilet seat, perching stool to assist with personal care.
- Progression of mobility from a walking frame to independence with the community physiotherapists.
- Support from an intermediate care team to assist with washing and dressing or meal preparation.
Your therapist and the ward will keep you updated but feel free to ask questions regularly as staff appreciate that this might be an anxious time. Please remember, you will not be sent home until the doctors, nurses and therapists think you are ready.









