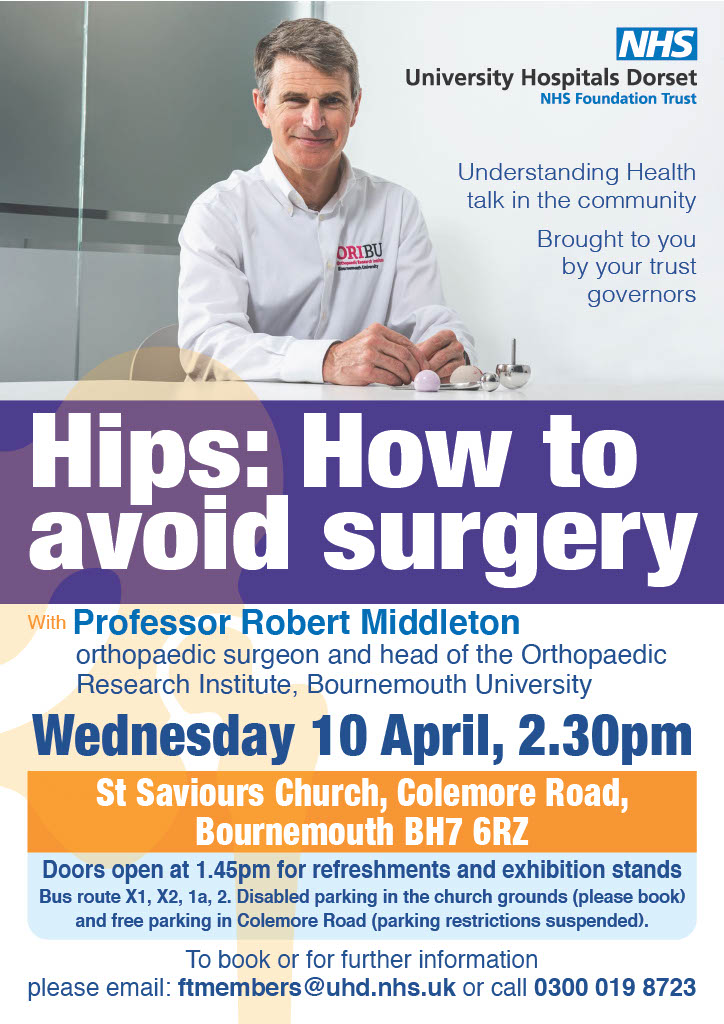
Understanding hips: how to avoid surgery
|
Join Professor Robert Middleton, consultant orthopaedic surgeon, in this community health talk on 10 April, brought to you by your trust governors. |
Understanding health talks 2024Three new Understanding Health Talks have been booked for the first half of 2024. This year the talks will be joint events with Bournemouth University and will have presenters from both organisations. These events are expected to be very populart so booking early is advised. To reserve your please, see below: Understanding Menopause ...with Rosie Harper, clinical specialist physiotherapist in pelvic health at UHD, and Dr Emma Thurston, senior lecturer in physician associate studies at Bournemouth University and GP with a special interest in women’s sexual and reproductive health. Wednesday 6 March 3-4pm Bournemouth Gateway Building, Lansdowne (Room BG-110) Understanding Concussion in Sport and Practice ...with Dr Keith Parry, head of department for sport and event management, and Osman Ahmed, senior physiotherapist at UHD. Thursday 2 May 4-6pm The Share Lecture Theatre in the Fusion Building on Talbot Campus
Understanding Pathology: Health under the microscope ...with Nathan Bourne, biomedical scientist and governance and quality manager at UHD, and Dr Anna Mantzouratou, FIBMS, FHEA principal academic in human genetics and program leader BSc (Hons) biomedical science life and environmental sciences department. Tuesday 4 June 6-7pm The Share Lecture Theatre |
Patients benefit from tattoo-less treatments
Thousands of patients receiving radiotherapy at University Hospitals Dorset no longer need to have permanent tattoos to accurately mark the target site for their treatment.
Radiotherapy involves a beam of radiation aimed at a tumour to kill it. As it can damage non-cancerous cells, the procedure involves complex planning to ensure the right dose is delivered at the exact site it is needed, with a series of small tattoos traditionally used to help guide this.
However at Poole Hospital, patients are now treated on one of three ‘surface guided’ radiotherapy treatment systems which use a series of cameras and image sensors to create a skin map of the individual patient instead. Combined with detailed treatment planning scans, a target site is 'locked' so if a patient – and their tumour – moves, it turns off the beam.
David Frost, head of therapy radiography at UHD, said: “One of our trust values in ‘always improving’, and here at UHD we are using the latest technology to do that for the benefit of our patients. While the tattoos assisted our treatment, they often had a negative psychological impact on our patients and were a permanent physical reminder of being unwell. For some of our patients it was also the first tattoo they ever had.
“This surface guided technology is quicker, more accurate and can allow a reduced imaging dose for our patients, reducing the level of radiation. Going tattooless is a fantastic milestone for all of us to reach.”

Patient Ola, with the radiotherapy team
The tattoo-less treatment is not commonplace in the NHS, and in many parts of the UK can only be offered in private centres. UHD is the first trust in the south west to offer the service, and the team also manages a fourth system from The Robert White Centre at Dorset County Hospital, in Dorchester. The centre is named after multi-millionaire businessman Robert White, who gifted Poole Hospital more than £10m to advance cancer treatment in the county before his death in 2015.
While the trust has been using the surface guided radiotherapy for two years, the team has gone tattooless for all cancers for the first time.
Ola Williams is one of the patients benefiting from the new treatment. He said: “Having cancer can be really unsettling and while you feel grateful for the treatment, it feels really positive not to have to go through another process – in this case having a tattoo.”
UHD carries out around 25,000 radiotherapy treatments each year, and the team supports around 130 patients every day. Some 210 new patients start their treatment every month, attending the department for five treatment session each week.
Josh Naylor, physicist in the department, said: “We get to know our patients really well during the course of their treatment and the feedback has been really positive. We’re really proud to be able to offer this to them and look forward to more improvements that benefit our patients in the future.”
Volunteers needed for hospital cancer care initiative
University Hospitals Dorset (UHD) is looking for volunteers to join an innovative cancer care project and support people on their cancer journey.
The new pilot, funded by Wessex Cancer Alliance, is recruiting volunteers to support people undergoing cancer treatment.
Volunteers may include former patients who have been directly affected by cancer, or friends and family members of those who have been impacted by cancer and want to make a difference.
Volunteers will be based with UHD’s cancer specialist teams across Royal Bournemouth and Poole hospitals, with referrals made where clinical teams feel a patient could benefit from additional health and wellbeing support via telephone or face to face, for an agreed period of time.

Jackie and Janet, two of UHD's volunteers
Claire Smith, Lead Cancer Nurse at UHD, said: “This is a really rewarding role that is about supporting patients during their cancer care and treatment. By providing advice, friendship and solidarity to someone throughout one of the hardest times of their life, volunteers are able to make a tangible and lasting difference through their lived experiences. In return, volunteers can expect to receive comprehensive training and support, and be a welcome addition to our hospital community.”
To find out more, email This email address is being protected from spambots. You need JavaScript enabled to view it. or get in touch with our volunteer services on This email address is being protected from spambots. You need JavaScript enabled to view it. if you have any questions.
National Cancer Patient Experience Survey
At the NHS, we want our patients to have the best experience possible, and having continuous patient feeback is crucial in helping us deliver what patients want and need.

The national Cancer Patient Experience Survey (CPES) asks for feedback from cancer patients (16 years and over*), to inform and improve local cancer services across England. Those who were treated for cancer as an inpatient or day-case, and left hospital in April, May or June 2023, will be invited to take part in the survey.
The survey takes no more than 20 minutes to complete and can be done online, on paper, or over the phone. If you need support completing the survey or need it made available in another language, you can call the free helpline number: 0800 103 2804.
The NHS and cancer charities use the results to understand what is working well and which areas need improvement. The results enable them to identify national and local priorities and work with patients and partners to deliver change.
The survey is anonymous, and all personal details will be kept safe.
The results of the survey will be available in Summer 2024.
For more information on the survey and how to access help and support in completing it, please visit www.ncpes.co.uk
*For those aged 16 and under, feedback is collected via the Under 16 Cancer Patient Experience Survey: www.under16cancerexperiencesurvey.co.uk












