New way for patients to connect with their care is coming
A new way for patients at University Hospitals Dorset (UHD) to be more connected with their care is coming this autumn.
The UHD Outpatients Portal is a secure online information and communication resource for patients under the care of the vast majority of UHD's specialist services.
Patients will be able to:
- receive appointment reminders by text message via their mobile phone
- view appointment letters digitally
- view clinic information about their upcoming appointment
- add their appointment to their personal calendar on their device, and
- view all upcoming appointment details and letters in one place.
Patients due to attend an outpatient appointment from this autumn will receive a text message from +44 7860 039092 which will include their appointment reminder and a link to access the portal. To access the portal, patients will simply need to confirm some demographic details or use their existing NHS log in details, if known. For younger patients, the message will be sent to their existing primary contact, usually a parent or carer.
The new service aims to improve patient access to information about their care, reduce the number of appointments missed each year through the use of timely reminders, increase the time outpatient teams have available to spend with patients who need their support the most, and reduce postal and administration costs for the hospitals. It's also better for the environment.
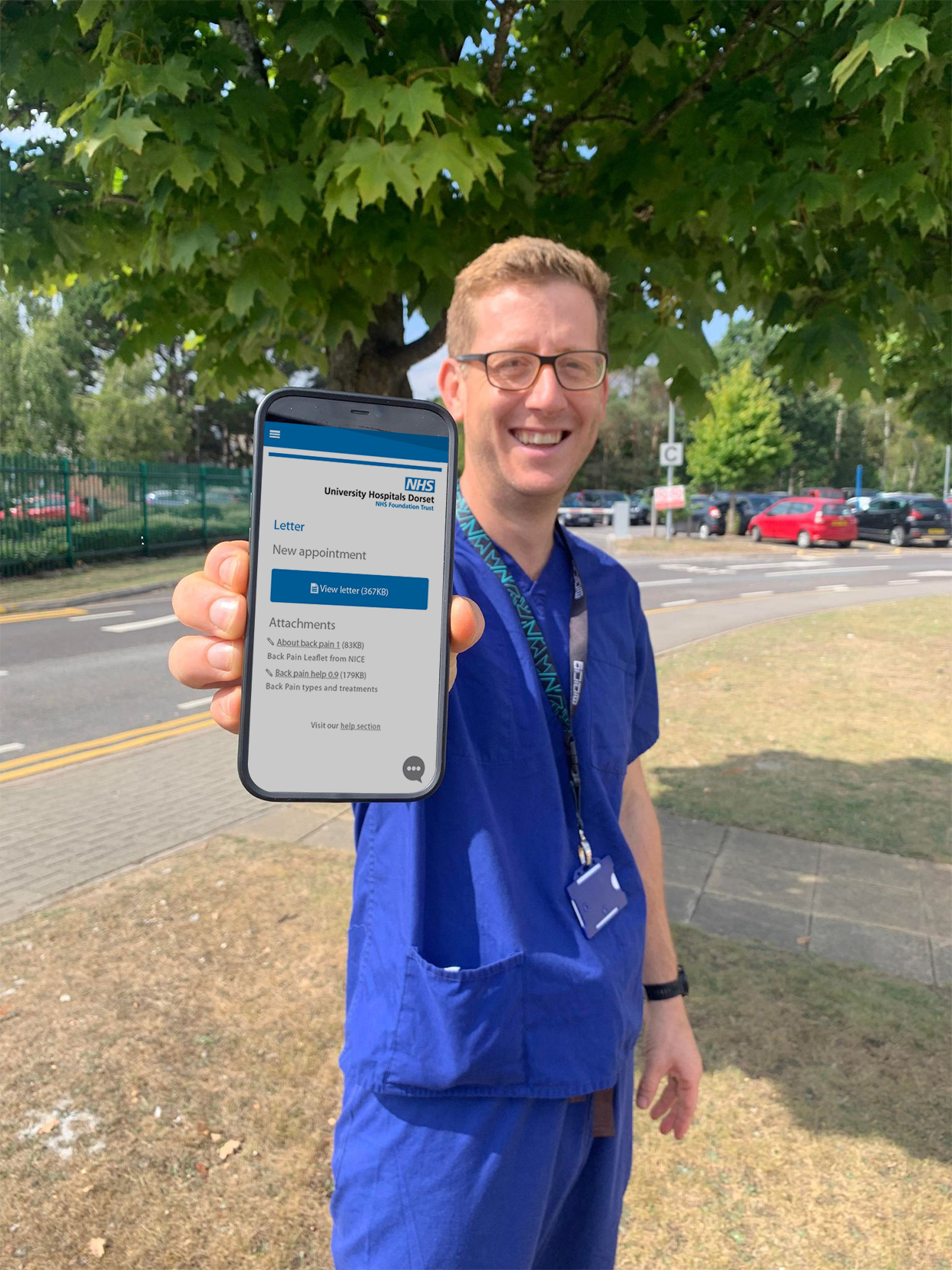
"This is a great step forward to support patients to be better connected to their care," said Dr Jonathan Marks, clinical director for outpatients services at UHD (pictured).
"Many of us choose to do our banking or shopping online securely, and it makes sense to take this approach to our health information too.
"Having all the details you need at your fingertips increases convenience, and should mean things like missed appointments or misplaced letters will be significantly reduced.
"We know from experience that when patients feel more connected with their care, their health outcomes are better."
UHD is working with DrDoctor, a company which has helped many trusts launch similar services and who are also supporting NHS Digital, the team behind the official NHS app.
What do patients need to do?
It's essential that UHD holds up-to-date patient contact details, especially mobile phone numbers – patients can check we have the latest details with the reception team at their next outpatient appointment.
Patients may also wish to add +44 7860 039092 to their phone address book so it's clear when messages from the outpatients team arrive.
Opting out
Patients who do not want to use the text messaging or online system can continue to be contacted by letter only and can telephone the call centre to rearrange your appointment.
While it is hoped most patients will appreciate the convenience, speed and security of the portal, it is simple for those who wish to opt out to do so. Simply click the link sent in your text message, or call the outpatients team. Patients who opt out will continue to receive letters, and be able to reschedule or decline appointments by phone.
Hospital dermatology team highly commended by British Medical Journal
University Hospitals Dorset’s dermatology team has been highly commended by the prestigious British Medical Journal (BMJ), coming in second place at its national award ceremony.
The team was praised for creating a system for patients to electronically add photographs to their medical records, which were then examined by a consultant without the need to come into the hospital. The service was set up at the start of the pandemic and ensured all patients who needed to be ‘seen’ within the two-week target were seen, with 66% being managed completely remotely.
The team worked closely with the IT department to create the solution and the image transfer service was set up in just three weeks. Once the images were uploaded by the patient, a consultant would then determine whether the patient needed to come in for a follow-up appointment, or be booked directly in for surgery.
Dr Anjnee Shah, dermatology registrar said: “At the start of the pandemic the dermatology service was already incredibly busy, and the team foresaw social distancing measures and an apprehension around coming into hospital would cause further strain.
“The service meant that patients didn’t have to be physically seen unless it was necessary, but we still ensured our patients received high-quality care.”
As well as meeting the two-week referral target, 56% of the patients seen virtually were directly listed for surgery, reducing the need for multiple appointments and added footfall in the hospitals.
The service also benefited trainee doctors who would have been missing out on training opportunities due to the pandemic. Trainees were able to review cases alongside consultants without breaking social distancing guidelines, allowing for valuable learning to continue within the department.
Dr Shah said: “Being recognised by the BMJ for our work throughout the pandemic is truly something to be proud of.
“We are so grateful to have the opportunity to celebrate the hard work and dedication the whole dermatology team has put in over the past 18 months to maintain the service, meet increasing demand and support local dermatology services.”
Poole Hospital celebrates 25 years of specialist menopause service
“It’s brilliant that more women now have the confidence to speak up about the menopause and how it has affected them.”
So says Mr Tim Hillard, consultant gynaecologist and menopause specialist, looking back on 25 years of Poole Hospital’s specialist menopause clinic. The clinic was one of the first of its kind outside of London and remains the biggest menopause clinic in the south west. “We are proud we have been offering this service for so long as while primary care provides support for many women there has always been a need for specialist care for the more complex problems,” explains Mr Hillard.
Menopause affects all women, with one in three experiencing significant health problems associated with the symptoms of menopause.
“Dealing with menopausal symptoms can have a major impact on a woman’s quality of life, their ability to balance work and family, and can lead to feelings of distress and an inability to cope,” said Amanda Hillard, menopause nurse specialist. “I know of women who have had to leave their jobs as they have felt unable to cope or discuss the severity of their menopause symptoms with their employer”.
Menopause symptoms include hot flushes, night sweats, vaginal dryness, reduced sex drive, pain with sex, difficulty sleeping, low mood and anxiety, brain fog and reduced memory all of which can have a serious effect on a woman’s mental health. The average age of the menopause is around 52, but many women start experiencing their symptoms in their mid to late 40s. Some undergo their menopause much earlier which can affect fertility options and increase long-term health risks.
The team treats women who are experiencing debilitating menopausal symptoms that the standard treatments such as hormone replacement therapy (HRT) are not alleviating. They also help patients experiencing early menopause, those with more complex medical problems and those who cannot necessarily take HRT such as women who have had breast cancer.
Since being established 25 years ago the team has moved from St Mary’s Maternity Hospital to the Harbourside Gynaecology Unit and expanded to include consultant Miss Elizabeth Stephenson. The service is now busier than ever, with 16 menopause clinics running every month. Not only do the team treat menopause, but the clinic is the principle regional training centre for Wessex providing education to other healthcare professionals including practice nurses, GPs and trainee gynaecologists.
Alongside educating healthcare professionals Amanda emphasises the importance of wider education on menopause in the community: “We work exceptionally hard to educate women so that when menopause happens, they know what to expect and where they can get support. But it’s not just women who are close to the expected age of menopause that need to be educated, it is younger women, their partners, employers and their teams of staff.”
Mr Hillard advises women to speak up and seek advice if they have any concerns around the menopause: “I would advise any woman who is experiencing problems around the menopause, no matter what stage of life they are at, to seek help and advice. Quite often symptoms can be alleviated through simple changes such as dietary and lifestyle alterations but there are also a variety of treatment options available if needed.”
In the first instance women who need support with menopause can seek advice through their GP and practice nurses, but if they are having further difficulties a referral can be made to the menopause clinic. General menopause advice can also be found at www.womens-health-concern.org.uk and www.menopausematters.co.uk









