Vital maternity service celebrates first anniversary
A maternity team at University Hospitals Dorset NHS Foundation Trust (UHD) has commemorated one year of supporting new parents and families.
The group of midwives, known as the Meadow Team, work together to provide consistent care for women from the global majority throughout their pregnancy, birth, and the postnatal period.
Their main aim is to ensure expectant mothers are seen by the same midwife, or a small group of familiar midwives, across all stages of their pregnancy. This is key to continuity of care, and for allowing the midwife to better understand an individual's needs and preferences.

The same team of midwives are also on-call for women during their labour and month, and their care and support is extended into the postnatal period with home visits for up to a month.
One mother who used the service praised "the warmth, care, and respect" during her care.
"I felt so supported whilst managing gestational diabetes, and I really appreciated the proactive approach of the team towards the end of my pregnancy, which I found very difficult", she said. "I felt safe and listened to; it was professional care at its peak."
The team support women who choose to give birth at home, in birth centres, or hospital settings depending on what is safest and appropriate for each individual. They also provide monthly face-to-face education classes, which is a great opportunity for expectant parents to meet other midwives in the team.
Midwives are either based at the Royal Bournemouth Hospital or Boscombe Children's Centre, and provide at least two home visits during pregnancy.
Elena Gray, continuity midwife and deputy lead of Meadow Team said: “We absolutely love what we do, being able to build genuine, meaningful relationships with the people we support. It creates an opportunity to truly understand women's values and preferences, enabling us to advocate more effectively and tailor care to their needs.”

Nurse-led Clinic to reduce cholesterol levels achieves international recognition and £350,000 funding boost
A clinic led by nurses from the Cardiology Team at University Hospitals Dorset has seen remarkable results for patients needing to reduce their cholesterol levels.
The Secondary Prevention Lipid Clinic supports those who have experienced a cardiac event and has focused medication optimisation and dedicated patient education.
In just six months, 72% of patients have reached cholesterol levels below national targets, a figure that far surpasses the typical 30-40% improvement seen over a 12-month period.
Anthony Young, UHD Lead Cardiac Advanced Clinical Practitioner, said: "The nurse-led Secondary Prevention Lipid Clinic has shown that by supporting patients with education about their cholesterol levels and educating them on secondary prevention, optimising medication for lowering cholesterol and ensuring we take a vested interest in their health, we have been able to lower cholesterol in 72% of patients after six months to below the current recommended targets. This not only improves the health of our patients but reduces the cost on the NHS over 5-10 years."
The team’s achievements were recently recognised on an international stage at the ESC Preventive Cardiology Conference in Milan, where they had the opportunity to showcase their work and engage with cardiovascular professionals from across Europe.
Additionally, the clinic has been awarded a £350,000 grant by the British Heart Foundation to support the expansion of secondary prevention of cardiovascular disease in east Dorset. This funding will enable collaborative work with three local Primary Care Networks, allowing the team to extend their reach and optimise cholesterol management for even more high-risk patients in the region.
This successful service has also been strongly supported by UHD Consultant Cardiologist, Professor Christopher Boos, whose guidance and encouragement have been instrumental in enabling the nurse-led team to pursue and achieve such outstanding outcomes.
Professor Boos said: “This is a considerable grant which is to my knowledge one of the first of its type to given in the UK. It has the genuine potential to transform the delivery of this novel nurse-delivered lipid lowering secondary prevention service across east Dorset. Its clinical impact is likely to be considerable. The wider implementation of this service is expected to significantly reduce secondary atherosclerotic cardiovascular events for patients with conformed significant coronary artery disease in our catchment.”
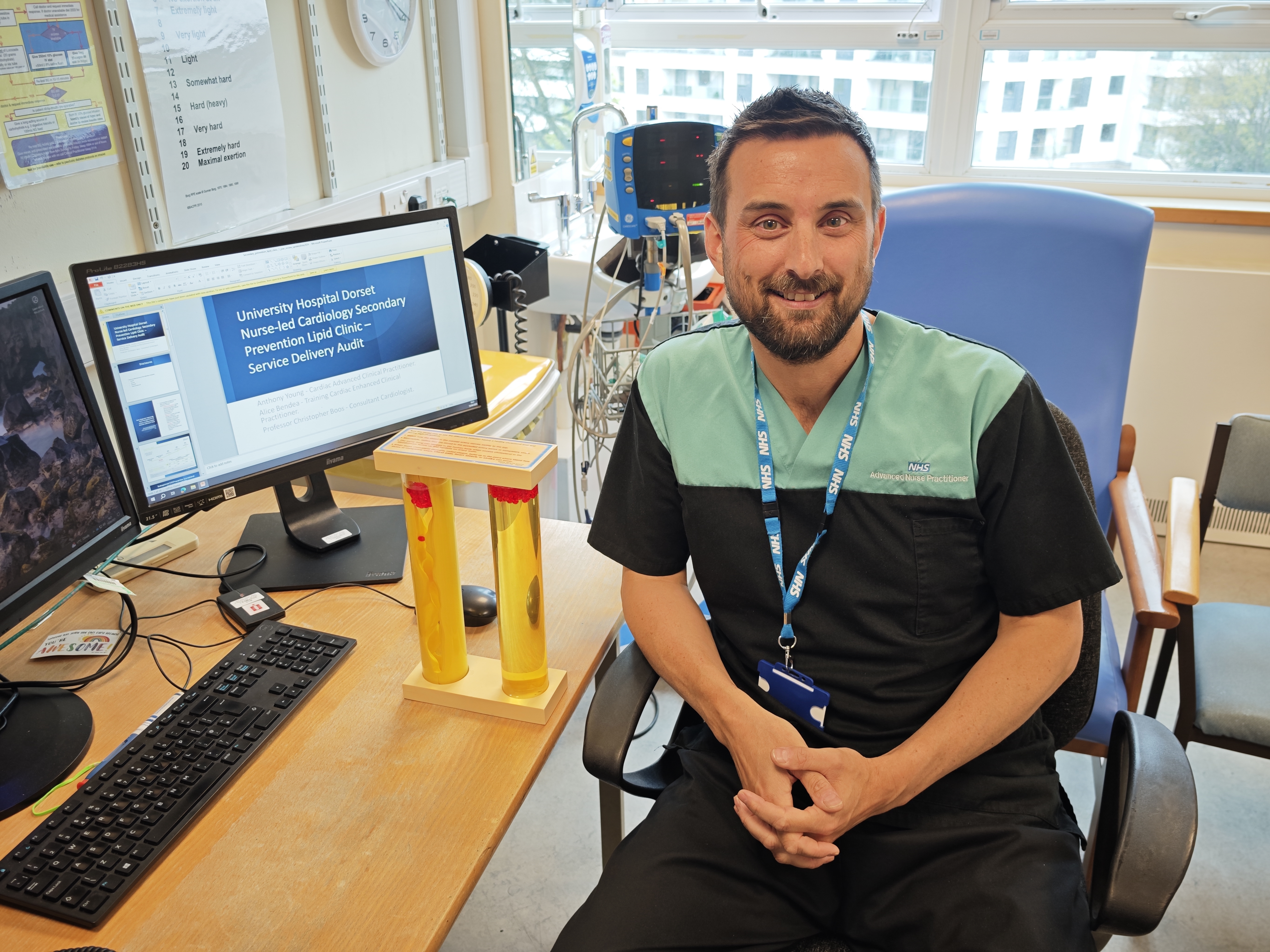
Anthony Young, UHD Lead Cardiac Advanced Clinical Practioner
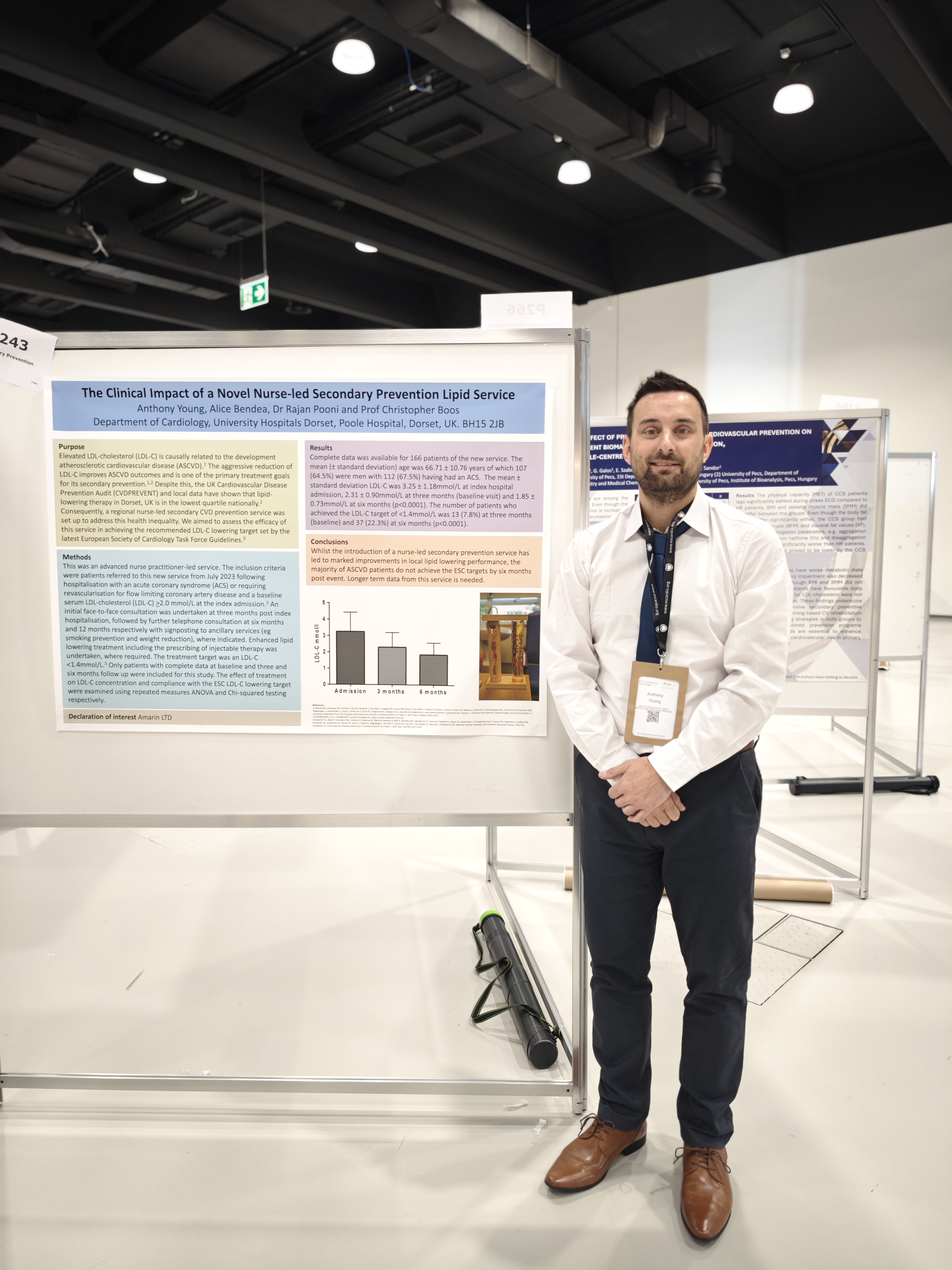
Anthony Young, UHD Lead Cardiac Advanced Clinical Practioner presenting in Milan.
Staff shine bright at hospital awards
Uplifting examples of inspiring care, teamwork and leadership were all celebrated at University Hospital Dorset’s (UHD) third annual awards on Tuesday.
More than 360 members of staff and hospital volunteers attended the event at The Pavilion in Bournemouth on 20 May to hear how the finalists were placed in each of 14 categories. They were also joined by patients and the local community who put forward staff for recognition.
The awards scheme received over 900 nominations, giving the judging panel a real challenge and shining a spotlight on the amazing work across UHD.
Chief Executive, Siobhan Harrington, said: “The awards are a fantastic opportunity to recognise the incredible teams across our Trust. Their hard work and commitment are invaluable.
"During this period of transformation, it's great to be able to come together and celebrate all that is great about UHD. We all come to work to provide the very best care for our patients, and special events like this give us an opportunity to recognise the impact we have.
“A huge thank you to all patients and colleagues who made a nomination, and to our UHD NHS Charity, Locum’s Nest and IHP for supporting this brilliant evening.”

Celebrating success: Dorset Apprentice of the Year 2025 (Degree category) awarded to Sarah Matthias
We are delighted to share the news that Sarah Matthias, Advanced Clinical Practitioner (ACP) in the Bariatric Surgical Service, has been awarded the prestigious Dorset Apprentice of the Year 2025 – Degree category, following the successful completion of her Master’s in Advanced Clinical Practice earlier this year.
Sarah, a dietitian by background, has embraced the transition into advanced practice within the surgical directorate, navigating the complexities of stepping into a role traditionally underrepresented by Allied Health Professionals (AHPs). Her journey has required not only clinical excellence but also resilience, leadership, and the courage to challenge professional boundaries.
"Sarah’s achievement is richly deserved. Her professionalism and vision for patient-centred care have brought tangible improvements to our service. She is an exemplar of what advanced practice can offer when supported and enabled across professional boundaries."
— Mr. R Byrom, Clinical Director for Surgery and Bariatric Surgeon
“I’ve had the privilege of supporting Sarah throughout her ACP journey, and I honestly don’t know how she’s achieved all she has while working full time and raising two children, her dedication has been genuinely impressive.”
— Melanie Crick, Clinical Supervisor and Colorectal Cancer Specialist Nurse
Reflecting on her award, Sarah said:
“The journey into advanced practice has been both challenging and transformative. It’s a privilege to represent dietetics and demonstrate the value of AHPs in surgical care. I hope my experience encourages others to explore advanced roles and drive positive change forward.”
We would like to congratulate Sarah on this outstanding achievement, which not only recognises her personal commitment but also showcases the impact of integrated, advanced clinical practice across the wider healthcare system.

Outpatients Assessment Clinic (OAC) - 'Think Big'
University Hospitals Dorset (UHD) has relocated its Outpatients Assessment Clinic (OAC) to the former St Mary’s Maternity Unit in Poole, following confirmation that its current location in Beales department store in the Dolphin Centre has closed.
Originally launched in December 2021 as part of UHD’s innovative ‘Think Big’ initiative, the Beales clinic was developed in response to the Covid-19 pandemic. It brought outpatient services into the heart of the community, significantly reducing waiting times and easing pressure on hospital sites.
Mark Mould, Chief Operating Officer at UHD, said:
“When we opened the Beales clinic, we were responding to unprecedented demand in the wake of Covid.
“Using lessons from the Nightingale hospitals, we created a high-quality, flexible outpatient space outside the traditional hospital setting.
“Since then, the clinic has gone from strength to strength – with over 75,000 patients seen across 19 specialties.
“While it’s bittersweet to say goodbye to a site that’s served us so well, we’re excited to welcome patients to our new facility at St Mary’s, with the intention to continue to ‘think differently’ on how we provide clinical outpatient services.
“Our fantastic staff and volunteers have been key to the clinic’s success, and their commitment will ensure we maintain the same high standards as we transition to the new location.”
The new clinic at St Mary’s will continue to provide vital outpatient services including abdominal aortic aneurysm (AAA) screening, dermatology, dexa scans, ophthalmology, orthopaedics, phlebotomy and ultrasound. It opened to patients from Thursday 5 June, with clear signage and volunteer support in place to assist visitors.
Core breast screening services previously delivered at Beales will now be enhanced at Poole Hospital, with remaining facilities relocated to another UHD site.
Watch this video to hear from the team about the big day and what the move to St Mary’s means for our patients: https://youtu.be/BDzhVNkX1pY.









