Patient information and support
Useful links
- Radiotherapy UK (RTUK) patient and families' hub
- Macmillan Cancer Support
- Prostate Cancer UK
- Wessex Cancer Alliance
- Respire (DIBH Coaching Patient Support)
Local support services
- Counselling service
- Wessex Cancer Support
- Patient Experience
- Look Good, feel Better
- Cancer services
- Citizens Advice Macmillan Cancer Advisors
- Prostate Cancer UK Peer to Peer Support
LGBTQ+ support
Side Effects of Treatment
It is important to note that radiotherapy side effects will vary from person to person.
Radiotherapy can cause both short and long-term side effects.
The side effects that you might expect will be detailed on your individual consent form and on the information leaflet that you will receive at the pre-treatment planning appointment. We will offer you a copy of this form if you do not have one.
You can find out more about general side effects here.
Radiotherapy Patient Information Leaflets
You will be given a radiotherapy information leaflet specific to your type of treatment when you attend for your radiotherapy planning appointment.
Note: We are currently in the process of adding radiotherapy patient information leaflets to the hospital website.
You will find some select radiotherapy patient information leaflets here.
If you would like to request a leaflet which not currently listed on the website, please contact the bookings team.
Eating Well with Cancer
Some types of radiotherapy for example, radiotherapy to the head and neck or oesophagus, can cause problems with eating and weight loss. For more information on this click here.
After Your Radiotherapy Treatment
Short term radiotherapy side effects can continue for around six weeks after finishing treatment.
Continue to follow any advice you have been given until the side effects settle.
If you have any general concerns regarding side effects or need further advice about radiotherapy aftercare, you can telephone the Dorset oncology and radiotherapy advice helpline (DORAH).
For urgent advice please call the oncology patient hotline.
Radiotherapy helpline (DORAH) – For non-urgent advice
Tel: 0300 019 2481
The Dorset radiotherapy helpline (DORAH) is for any advice about any radiotherapy treatment you have had. It is open between 8am and 5.30pm, but a message can be left at any time. It is important to note that the DORAH helpline is not for emergencies.
Oncology patient hotline - for urgent advice
Tel: 07917 655 889
This number can be used at all times of the day or night for urgent inquiries. In the event your call is not answered, please leave a message stating your name, hospital number, and contact telephone number. You should be contacted by a nurse within 30 minutes. In the unlikely event that you are not called back within 30 minutes, please call again.
Radiotherapy Treatment
When you arrive at level minus 2, pink zone please bypass the electronic check-in, and the first oncology outpatients' reception desk.
Make your way to the radiotherapy reception desk.
Once you are checked in, you will be directed to the main radiotherapy treatment waiting area.
Note: If you have been asked to complete any pre-treatment preparation, ie. Bladder or Bowel preparation, we ask that you check for any appointment delays before you start. Then please follow any instructions given at the planning appointment.
For any queries relating to preparation, please speak to a member of staff when you arrive.
The radiographers will call your full name over a Tannoy (loud speaker) and ask you to come to a specific sub-waiting area. You will be called in for treatment when it is your turn. If you are in a wheelchair, or don't hear your name called, please don't worry, we will come to find you.
To help us to keep to time and ensure clothing is not obstructing our procedures, you will be asked to change into a gown. You will need to remove all clothing covering the area of the body we are treating. You can bring your own long dressing gown if you wish. There are changing areas available in all areas.
If you need any clarification on whether you need to change, what clothing to remove, or if you need directions to the changing areas, please ask any member of staff.
Therapeutic Radiographers.
In Poole hospital we have 3 treatment machines (linear accelerators – or linacs) all named after landmarks called Chesil, Furzey and Shell Bay. In Dorchester, at the Dorset county hospital we have 1 radiotherapy linac machine called West Bay. The machine you will be on will be printed on your appointment list.
All 4 machines are Varian Truebeam Linear Accelerators and look like this:

We also have a superficial radiotherapy machine called Durdle. You may be booked on this machine if you have a superficial skin cancer.

Each appointment will take between 10-30 minutes. For most of that time the therapeutic radiographers will be getting you in the same position as you were in for your planning appointment.
SGRT (Surface Guided Radiotherapy) is an advanced form of technology used on our linear accelerator (linac) treatment machines at UHD. It allows us to position you accurately without the need for permanent tattoos on your skin. When getting you in the correct position for your treatment, you may see a harmless red light projected onto your skin. You can close your eyes if you wish.
Once we are happy with your position, we will leave you alone and go next door to the control room. There may be a period where nothing seems to be happening. This is where we are making our checks and getting the machine ready. We will watch you on CCTV. You will be given instructions on how to call for help if required.
Before the treatment begins, we will use the treatment machine to take some 3D pictures of your internal anatomy (CBCT). We compare these pictures against your planning CT scan to check that your treatment will be given accurately. If tiny micro-adjustments are required to make your treatment more accurate, you may feel and hear the couch moving slightly.
When we are happy that the treatment will be accurate, we will switch on the treatment beam. You will not feel anything during the delivery of radiotherapy as it is an x-ray treatment. You might hear a buzzing noise when the treatment beam is on. Surface guided technology means that we can monitor your position closely throughout each treatment. The machine will automatically switch off if you are out of position at any time.
If you are booked on Chesil, Furzey or West Bay, the treatment machine will move around you under our guidance. It will not touch you.
If you are having radiotherapy on Durdle, the radiographers will place the machine gently, but firmly in direct contact with the skin for the duration of the treatment. Treatment on Durdle can take around 1-10 minutes but you will be in the room for around 20 minutes.
You will be monitored closely by your therapeutic radiographers. You will be asked how you are getting on and you can let us know if you have any questions or if you need help to manage side effects at any time. We can also arrange for you to be seen by a specialist radiographer, consultant or other specialist team should you have any problems during your course of treatment. Please don't suffer in silence – we are here to help you!!
Unless you have been informed otherwise, you will receive a follow-up appointment to see a consultant, review radiographer or consultant radiographer. Typically, this will be 4-6 weeks after completion of your radiotherapy course. If you need help and advice between the end of radiotherapy finishing, and your follow-up you can find our helpline information here.
Brachytherapy
What is Brachytherapy?
Brachytherapy is a type of radiotherapy treatment that involves placing radiation inside the body. This allows a high dose of radiation to be delivered to the tumour, while minimising damage to the surrounding healthy tissues. It may be used as a stand-alone treatment or sometimes in combination with external radiotherapy and chemotherapy. The radioactive source is either a permanent implant (Low Dose Rate - LDR) and the treatment delivered over a period of weeks, or a temporary implant (High Dose Rate – HDR) where the treatment lasts a few minutes. Some procedures require a general or spinal anaesthetic, while others can be given on an outpatient basis.
Brachytherapy treatments offered at UHD:
- LDR Prostate Brachytherapy
- HDR Prostate Brachytherapy
- HDR Cervix Brachytherapy
- HDR Vaginal Vault (post-surgery) Brachytherapy
The Brachytherapy Team
The team is made up of different professionals including:
- Therapeutic Radiographers
- Medical physicists/clinical scientists
- Bookings officers
- Dosimetrists
- Consultant Clinical Oncologists
Useful Brachytherapy contacts
Please use the number below for any brachytherapy related queries:
Brachytherapy office number – 0300 019 2047 (answerphone)
Patient information leaflets
Information leaflets for the different brachytherapy treatments offered at UHD can be found below. You may have already received a paper copy. Prior to your treatment, the brachytherapy radiographers will provide further information on your specific treatment.
Prostate Brachytherapy leaflets
- Low dose rate prostate brachytherapy service
- Prostate brachytherapy service HDR (high dose rate)
- Information regarding prostate brachytherapy preparation
Gynaecological Brachytherapy leaflets
Planning your treatment
Preparing for your planning appointment

The therapeutic radiographers use a planning CT scanner to collect detailed pictures of the treatment area. This information is used to ensure that we target the precise area for treatment. Although it may seem similar, this scan is not the same as any previous CT scans you may have had for diagnosing your conditions. The planning scan can be used in conjunction with previous diagnostic scans to help us to precisely plan your radiotherapy treatment. You will not normally get any results from this planning scan.
For some procedures, we will ask you to follow specific instructions prior to your first visit. You will be informed about any preparation in the first letter from us, or over the phone. Please ensure you follow any instructions given to avoid unnecessary delays.
How long does the planning take?
Please allow 2-3 hours for your planning appointment. If you plan to drive to the planning appointment, we recommend that you do not park on the side roads as these are only limited to 2 hours free parking.
The planning appointment
On arrival you will meet a therapeutic radiographer, apprentice or CT support worker who will explain the procedure and answer any questions. They will also reconfirm that you consent to the procedure.
Radiation can cause damage to an unborn baby. Therefore, if you are 55 years old or under, we must ask you to confirm that there is no possibility of pregnancy.
During the planning appointment the body part to be treated will need to be clear of jewellery and clothing. We will ask you to change into a hospital gown. We use surface guided technology so we will need to partially uncover you for the duration of your scan. But we will cover you as soon as we can.
We will need to position you in a specific way that can be reproduced for each future radiotherapy treatment. You will need to keep still for up to 20 minutes for your planning scan and for subsequent radiotherapy treatments so please let us know if we need to make you more comfortable.
Some patients may require an injection of contrast dye during the planning scan. If this is required for your scan, the radiographers will discuss this with you and insert a small tube (cannula) into the arm or hand prior to the scan. The cannula will be removed 20 minutes after the injection. We will ask you to drink some water before you leave.
Please be aware that we cannot use a power PICC or any type of central line to deliver contrast dye in this radiotherapy department.
See below for information on what you can expect depending on the specific area being treated.
Dental advice
If you are having radiotherapy which includes the mouth area you will have a dental check up before planning to assess your teeth. Some patients will need dental work completed before having radiotherapy planning and treatment. You will be informed by the head and neck team if this applies to you prior to receiving your radiotherapy planning appointment.
You will get a prescription for a special toothpaste and mouth wash which can be continued by your GP.
Keeping still for radiotherapy
When delivering radiotherapy to the head and neck it is important that the head is kept as still as possible for the duration of the treatment. To achieve this, we may need to make a mask (shell) to wear during your treatment.

A mask is made by heating a piece of flat plastic in a waterbath for a couple of minutes until it is warm and flexible. It is then stretched over the head and neck area and smoothed around your features. It takes a few minutes to dry and harden. The mask feels a bit wet and warm when it is made but you will be able to breathe normally through holes in the material.
Your mask must fit your face perfectly. If you have long facial hair, you can help us to make a well-fitting mask by trimming very short or by shaving off before your planning appointment.
You will wear the mask again for up to 20 minutes during each treatment.
Will I have an injection during the scan?
Most patients having planning for radiotherapy to the brain, head or neck regions will require an injection of contrast dye to be given during the scan.
If this is required, the radiographers will explain the process when you arrive.
The CT Planning Scan
You will need to lie on a special inclined board with arms raised above your head. It is important to continue with any arm exercises as recommended after surgery. This will help you increase your arm mobility and reduce muscle tension when we position you. If you're uncomfortable, let the radiographers know as soon as possible —they can adjust your position.
We will need to uncover your chest completely for this procedure as we use skin surface guided technology to ensure you are positioned correctly.
The planning scan itself will take around 15-20 mins.
Will I need to hold my breath?
We will ask you to try holding your breath for your scan if you are having radiotherapy treatment to the following areas:
- Left Breast
- Left Chest Wall
- Treatment to the internal mammary chain (IMC)
The radiographers will coach you to hold your breath for up to 20 seconds during your scan. If you are able to do this consistently for the planning appointment, you will be asked to do the same thing during the delivery of the radiotherapy treatment.
You can find videos and resources on the RESPIRE website which will help you to prepare.
Some patients are not suitable for a breath-hold technique (DIBH). If this is the case, we will discuss this with you at the scan.
Will I have an injection during the scan?
You will not have an injection during this scan.
Preparing for the planning scan
We will send you an appointment letter, or phone you at least 5 days in advance of the CT planning appointment with the required information if you need to prepare for the scan.
I have been told I need a full bladder and empty bowel for the scan. What can I do to prepare?
At least 5 days before your scan
- Drink plenty of fluids, ideally two litres a day (unless on fluid restriction). Water or squash is best.
- Try to avoid eating foods/ drinks which are known to make you gassy (eg baked beans, cabbage, spinach, fizzy drinks).
- Eat regular meals
- Drink and chew slowly
On the day of the scan
- Continue with good hydration. Drinking water regularly until your appointment.
- Eat a good breakfast/ lunch/ dinner (but continue to avoid gassy foods).
- Try to empty your bowels (have a poo) naturally before you leave for the department. Do NOT strain or force.
Prostate Cancer Specific Information
If you are having radiotherapy to the prostate area you can find additional information about how to prepare and what to expect here.
I have a problem with the preparation
If you have any problems with the preparation instructions given to you, or are not sure about what to do, please contact the bookings team for advice.
Will I have an injection during the scan?
Most patients having planning for radiotherapy to the pelvis will require an injection of contrast dye to be given during the scan.
If this is required, the radiographers will explain the process when you arrive.
Keeping you still during treatment is extremely important for accuracy of radiotherapy. How we position you and stop you from moving during treatment (immobilisation) will vary depending on where the cancer was found in your chest.
For cancers that are in the mid or lower chest
You will need to lie on a special board with arms raised above your head. If you have been given any arm or shoulder exercises then please continue with these. They will help you increase your arm mobility and reduce muscle tension when we position you. If you’re uncomfortable, let the radiographers know as soon as possible —they can adjust your position.
We will need to uncover your chest completely for this procedure as we use skin surface guided technology to ensure you are positioned correctly.
The planning scan itself will take around 15-20 mins but you may be in the room with us for longer.
For cancers that are in the upper part of the chest
We may need to make a mask (shell) to wear during your treatment.

A mask is made by heating a piece of flat plastic in a waterbath for a couple of minutes until it is warm and flexible. It is then stretched over the head, neck and upper chest area and smoothed around your features. It takes a few minutes to dry and harden. The mask feels a bit wet and warm when it is made but you will be able to breathe normally through holes in the material.
Your mask must fit perfectly. If you have long facial hair, you can help us to make a well-fitting mask by trimming very short or by shaving off before your planning appointment.
You will wear the mask again for up to 20 minutes during each treatment.
Will I need to hold my breath?
In most cases, we will not ask you to hold your breath for your planning scan, or radiotherapy treatment unless the consultant oncologist requests this technique.
If the breath hold technique is required, we will send you a preparation letter or phone you with more details. On the day of the planning scan the radiographers will coach you to hold your breath for up to 20 seconds during your scan. If you are able to do this consistently for the planning appointment, you will be asked to do the same thing during the delivery of the radiotherapy treatment each day.
You can find videos and resources on the RESPIRE website which will help you to prepare for a breath hold technique.
Some patients are not suitable for a breath-hold technique (DIBH). If this is the case, we will discuss this with you at the scan.
Can I eat and drink normally?
If you have a cancer of the lower oesophagus we may require you to “fast” (take no food or fluids) for 2 hours before your planning appointment. If this applies to you, we will contact you via letter or phone prior to your appointment to give further instructions.
Will I have an injection during the scan?
Most patients having planning for radiotherapy to the lung/ Oesophagus (Thorax) will require an injection of contrast dye to be given during the scan.
If this is required, the radiographers will explain the process when you arrive.
Keeping you still during treatment is extremely important for accuracy of radiotherapy.
You will need to lie on a special board with arms raised above your head. If you have been given any arm or shoulder exercises, please continue with these. They will help increase your arm mobility and reduce muscle tension when we position you. If you’re uncomfortable, let the radiographers know as soon as possible —they can adjust your position.
We will need to uncover your chest and abdomen and pelvis almost completely for this procedure as we use skin surface guided technology to ensure you are positioned correctly. We will cover your modesty.
The planning scan itself will take around 15-20 mins but you may be in the room with us for longer.
Will I need to hold my breath?
In most cases, we will not ask you to hold your breath for your planning scan or radiotherapy treatment, unless the consultant oncologist requests this technique.
If the breath hold technique is required, we will send you a preparation letter or phone you with more details. On the day of the planning scan the radiographers will coach you to hold your breath for up to 20 seconds during your scan. If you are able to do this consistently for the planning appointment, you will be asked to do the same thing during the delivery of the radiotherapy treatment each day.
You can find videos and resources on the RESPIRE website which will help you to prepare for a breath hold technique.
Some patients are not suitable for a breath-hold technique (DIBH). If this is the case, we will discuss this with you at the scan.
Can I eat and drink normally?
We may require you to “fast” (take no food or fluids) for 2 hours before your planning appointment. If this applies to you, we will contact you via letter or phone prior to your appointment to give further instructions.
Will I have an injection during the scan?
Most patients having planning for radiotherapy to the abdomen will require an injection of contrast dye to be given during the scan.
If this is required, the radiographers will explain the process when you arrive.
If you are having radiotherapy to a superficial area of your skin, a radiotherapy planning scan will not normally be required. This is called a Clinical Mark Up session.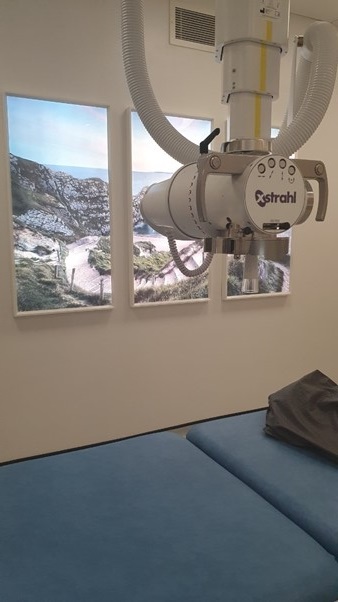
You will be lying down on a bed in a position that is comfortable for you.
The consultant will look at your notes and your skin and decide exactly what area needs treatment. They will draw temporary marks on your skin with a pen to define the treatment area.
The radiographers will take a template and photographs of the pen marks.
The radiographers will remove the pen marks before sending you home with treatment appointments and information.
The CT Planning Scan
For this type of scan we will contact you in advance to let you know if there is any preparation. When you are taken for your scan we will ask you to lay on our couch. You will need to be able to lay relatively flat however, we will be able to modify your position to make you as comfortable as is possible. We have a range of pads and mats that we can use for this purpose. If you're uncomfortable, let the radiographers know as soon as possible - they can adjust your position. You will need to be able to tolerate the position for around 20 minutes.
If you suffer with pain, please continue to take any regular pain medication before you come. If you have any top up pain medication prescribed to you such as oromorph, please bring this with you to your planning appointment.
For the scan we will need to uncover the area of the body that will need radiotherapy.
Can I eat and drink normally?
Unless we tell you otherwise, you will be able to eat and drink normally before this type of planning.
Will I need to hold my breath?
Unless we tell you otherwise, we will not normally ask you to hold your breath for this type of procedure.
Will I have an injection during the scan?
If an injection is required, the radiographers will discuss this with you on the day, before going ahead with the planning.









