Cardiac Rehabilitation
Cardiac Rehabilitation Exercises
These exercises are only to be attempted following guidance from the Cardiac Rehabilitation Team.
It is very important that you observe the following points when exercising.
DO NOT BEGIN OR CONTINUE TO EXERCISE IF:
- You have pains in the chest or legs
- You feel sick
- You have palpitations
- You are sweating excessively
- You feel dizzy
Let the course team know if you experience any of these symptoms during the course.
If you have been prescribed GTN spray or tablets, ensure you have them with you BEFORE you start exercising. If necessary, use the GTN as you have been previously directed. Remember to sit down before you take the GTN, this will help to reduce any dizziness you may have. If your symptoms don’t pass quickly do not hesitate to seek medical advice.
AVOID
- Allow 1.5 - 2 hours following a large meal
- Allow 1 hour following a small meal
- Allow half an hour following a snack
Exercising when you are unwell
- Exercising with a heavy cold or 'flu is unsafe. If you feel generally OK but have a runny nose without a 'chesty' cough, then you can exercise at a lower level than usual.
Exercising in extremes of temperature
- Hot or cold weather can affect your response to exercise. Avoid exercising in these conditions.
Competing with others
- Everyone has a different level of fitness and capability. Go at your own pace and NEVER try to compete.
NORMAL FEELINGS WHEN EXERCISING
When exercising it is desirable to feel:
- Slightly out of breath or have an increased depth and rate of breathing (However, you should be able to hold a conversation)
- A slight sweat or 'glow' to your skin (Some people sweat more than others)
- That your muscles have worked. Until you get used to the exercise you may find that your muscles ache, especially the day after. This aching is less likely to occur as you increase in fitness, especially if you adequately warm-up and cool-down.
- Feelings of well-being. A good indication of having exercised at the right level is if you feel pleasantly tired or slightly invigorated.
EXERCISE INTENSITY
In addition to using 'common sense' feelings, it is useful to be able to monitor how hard you are exerting yourself. Two ways of assessing the intensity of your activity are: Rating Exertion - The Borg Scale and Measuring the Heart Rate - Pulse Taking.
The Borg Scale
This is a numbered scale, with descriptions of intensity, where by you can 'rate' how hard you perceive the exercise to be. Everyone should initially learn to use the Borg Scale to assess how hard to work during the exercise session.
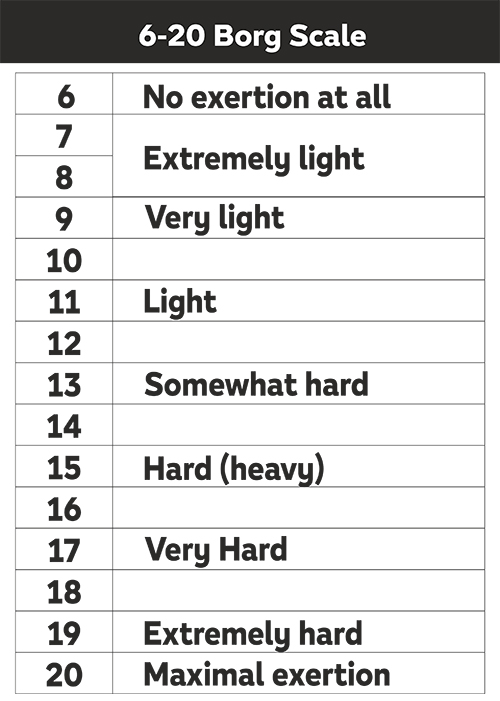
To gain the most benefit for your health, aim to achieve a score between 11 & 14 during the stamina part of the exercise session.
If you reach a score of 15 and above during the session you are pushing yourself too hard; slow down the rate at which you are doing the exercise, or choose the easier option for that particular exercise.
Standing exercises
Laura
(we apologise for the reduced sound quality due to wind noise)
Seated exercises
Laura
Cardiac Rehabilitation
Contact
Bournemouth Cardiac Rehabilitation: 0300 019 4515
Poole Cardiac Rehabilitation: 0300 019 2876
Monday to Friday 9am-5pm
Or email This email address is being protected from spambots. You need JavaScript enabled to view it.

Cardiac Rehabilitation
Advice and Education - Medicines for the Heart
What follows is basic information about some of the more commonly used medicines. The information provided has been selected for patient use. It is not intended to be comprehensive.
Aspirin
Whenever a blood vessel wall is damaged, certain cells (called platelets) collect around the area of the damage and clump together to form a clot. If the clot becomes too large it can block the blood vessel and prevent blood from reaching the heart muscle. This is what happens when you have a heart attack. Aspirin (in low doses) helps stop platelets sticking together, which prevents clots forming and prevents your new stent or bypass graft from blocking.
Aspirin can sometimes cause stomach irritation or heartburn. To reduce the risk of irritation, it is important that you take your aspirin with or just after food and dissolve it in water before taking it. If you do get indigestion with aspirin, you may find that the coated form of aspirin is better.
If you need to take a painkiller, avoid painkillers that contain aspirin, ibuprofen, naproxen or any other non-steroidal anti-inflammatory drug (NSAID). Paracetamol or Co-Codamol can be used instead. If you would like some help with choosing a suitable painkiller, ask your Pharmacist or local chemist.
Antiplatelets (e.g. Clopidogrel, Ticagrelor, Prasugrel)
Antiplatelets are similar to Aspirin as they also help to prevent platelets sticking together and forming a clot. Patients who have undergone an angioplasty with stenting, or who have had a heart attack will be given both Aspirin and one other, either Clopidogrel, Ticagrelor or Prasugrel. The Aspirin will usually be continued indefinitely and the Clopidogrel, Ticagrelor or Prasugrel for a set period of time; this will be stated on an antiplatelet card which will be given to you before discharge.
If you have a stent and there is any question of the Clopidogrel, Ticagrelor or Prasugrel being stopped by anyone, it must first be confirmed with your Cardiology Consultant at the hospital.
Notify your dentist if you are taking Clopidogrel/Ticagrelor/Prasugrel.
Please note: Whilst taking Aspirin/Clopidogrel/Ticagrelor/Prasugrel you may notice that you bruise more easily or if you cut yourself it takes slightly longer than usual to stop bleeding. This is quite normal but you are advised to see your GP if you have any concerns or develop any other unusual bleeding from any other areas, e.g. bowels.
Proton Pump Inhibitors (e.g. Omeprazole, Lansoprazole, Esomeprazole, Pantoprazole, Rabeprazole)
Proton Pump Inhibitors reduce the production of acid in the stomach, preventing or relieving irritation of the stomach lining.
Aspirin combined with another antiplatelet can irritate the lining of the stomach and, due to this action on platelets, may lead to blood loss. Omeprazole or a similar agent has been prescribed to reduce the likelihood of this happening. (see sheet on page 73 for secondary prevention guidelines)
The omeprazole (or similar agent) will usually be stopped on stopping your clopidogrel, ticagrelor or prasugrel. You may however continue on omeprazole (or similar agent) despite stopping clopidogrel, ticagrelor or prasugrel if you are likely to have or have previously had stomach trouble. This will be guided by your GP.
Statins (e.g. simvastatin, atorvastatin, pravastatin, rosuvastatin, fluvastatin)
Cholesterol is produced in the liver with the help of an enzyme. Statins block the effect of this enzyme and reduce the production of cholesterol. Statins reduce the levels of bad cholesterol (LDLs) and increase the levels of good cholesterol (HDLs).
It is recommended that people who have coronary artery disease take lipid-lowering drugs such as statins to reduce their blood cholesterol. Even if your cholesterol is not high, reducing it will lessen the chance of you having another heart attack or stroke.
Statins can cause stomach pain, wind, constipation or diarrhoea. If this happens to you, tell your doctor because reducing the dose may make this better. A rare but serious side effect of statins is inflammation of the muscles (myositis). You must tell your doctor if you have any unexpected muscle pain, tenderness or weakness.
Drinking grapefruit juice or eating grapefruit should be avoided if you are taking a statin drug called simvastatin. However, if you are taking another statin, such as atorvastatin, then grapefruit juice (or the grapefruit) can be taken in small quantities.
ACE Inhibitors (e.g. lisinopril, ramipril, perindopril, captopril, enalapril)
ACE inhibitors (Angiotension converting enzyme inhibitors) have several actions. They reduce blood pressure by dilating blood vessels and reducing fluid retention. Your heart is a muscle and after a heart attack will have suffered some damage, the heart will have to start to work harder to pump blood around your body. ACE inhibitors allow the blood vessel walls to relax and widen, reducing the work the heart has to do which reduces your changes of heart failure or a further heart attack.
Whilst you are taking ACE Inhibitors your GP will routinely arrange a blood test to check your kidneys are working well. This is particularly important when you first start this medication.
A dry, tickly cough can sometimes develop when taking ACE inhibitors. This is quite common and you should not worry about it. If it becomes troublesome you should speak to your doctor who can change you to a similar drug, called an angiotensin II receptor antagonist (or an ARB). The cough you had with the ACE inhibitor may take 3 or more weeks to disappear once the ACE inhibitor has been stopped. It is important NOT to stop taking them suddenly. Discuss any concerns with your GP.
Angiotensin II Antagonists (e.g. Candesartan, Valsartan, Losartan)
Angiotensin II receptor antagonists work in a very similar way to ACE inhibitors, reducing blood pressure and fluid retention, but do not cause the persistent dry cough that ACE inhibitors can sometimes cause.
Beta-blockers (e.g. atenolol, bisoprolol, nebivolol, carvedilol, metoprolol)
These drugs work by reducing the effects of adrenaline in the body. Adrenaline normally increases the heart rate and causes a rise in blood pressure. By blocking these effects, beta-blockers lower the work the heart has to do and therefore reduce the chance of you having angina, abnormal heart rhythms or experiencing a further heart attack.
Minor side effects are common and include tiredness and cold hands and feet. Other less frequent effects include nausea, diarrhoea, skin rashes, impotence or other sexual disorders, nightmares and pins and needles in the fingers.
It is important NOT to stop taking them suddenly as this may bring on angina and/or an increase in your blood pressure. Discuss any concerns with your GP.
Diuretics 'water tablets' (e.g. furosemide, bumetanide, bendroflumethiazide and others)
Diuretics control the amount of water in the body. They get rid of extra water and salt in your urine, and relieve congestion in your circulation.
You will need to use the toilet frequently for a few hours after taking these tablets so find a time of day that suits you. It is best to take diuretic tablets in the morning but if you are directed to take them twice a day, take your second dose at lunchtime or early afternoon.
If you have a special occasion to attend, where frequently visiting the toilet would be a nuisance, you can take the tablet at a different time that day.
It is important not to stop taking diuretic tablets without first consulting your GP, as missing even one dose could lead to fluid building up within the body.
Potassium Sparing Diuretics (e.g. eplerenone, spironolactone)
These are weak diuretics that increase the output of water, but prevent too much potassium being lost at the same time. This helps maintain the balance of salts within the blood. They do this by inhibiting the action of aldosterone, a substance produced within the body which controls your blood pressure and heart function.
Diuretics and potassium sparing diuretics are used to help manage the symptoms of heart failure.
Before you are started on diuretics or potassium sparing diuretics a blood test will check your potassium level and kidney function. Further blood tests should be repeated within the first week of starting,after a month, or after a change in dose.
Nitrates (e.g. glyceryl trinitrate tablets and spray, isosorbide mononitrate)
These work by widening coronary arteries and increasing blood flow through them, allowing the heart to get more oxygen.
Glyceryl trinitrate (GTN) comes as tablets or a spray and is used to relieve symptoms of angina.
How to use your GTN:
- If you get angina symptoms, stop what you are doing and rest. Sit down if possible
- If your pain does not ease within a minute spray one or two puffs, or place one to two tablets, under the tongue
- If after 5 minutes your pain has not resolved take a second dose
- If after 10 minutes (2 doses) you still have pain you should call an ambulance. You can continue to take your GTN every 5 minutes until the ambulance arrives
- With GTN tablets, once the pain has resolved either spit out, or swallow, the tablet. If you need to take a second dose, spit out the tablet and place another one under the tongue.
- If using GTN spray, once the pain has resolved rinse your mouth with water to remove excess spray (if possible).
Always carry your GTN with you. If you do not use your GTN very often, SIT DOWN before you take a spray as it can cause a rapid dilation of blood vessels making you feel lightheaded. Other side effects include facial flushing, dizziness or headaches. These will subside as the drug wears off. Paracetamol can be used to relieve the headache (do not use ibuprofen or aspirin).
If you find that you are increasing the amount of times you are using GTN, (on average greater than four separate occasions a day) make an appointment to see your GP as soon as possible. It may be helpful to make a note of what, if anything brought the angina on and if anything relieved it. This will help you give an accurate description of your symptoms to the doctor, thereby assisting their diagnosis. An angina/symptom record sheet may be found on page 74.
If you have been prescribed Sildenafil (Viagra), Tadalafil (Cialis) or Vardenafil (Levitra) leave at least 12 hours between taking one of these and using your spray, or if you take nitrate tablets, allow at least 24 hours (48 hours for Cialis).
Long-acting Nitrates (e.g. Isosorbide mononitrate, Isosorbide dinitrate)
These are tablets taken either once daily or twice a day to prevent attacks of angina. If you are prescribed this medication twice daily then the second dose should be taken no later than 4pm, this allows your body to have a 'nitrate free period' and reduces the likelihood of intolerance.
Initially they may give you headaches, but this usually settles as the body adjusts to the medication. If it is particularly troublesome problem then discuss this with your GP.
Do not take Sildenafil (Viagra), Tadalafil (Cialis) or Vardenafil (Levitra) whilst you are prescribed Isosorbide Mononitrate or Isosorbide dinitrate unless advised appropriately by your Cardiologist.
Anticoagulant medicines
Blood clots are made up of platelets (tiny blood cells clumped together) and a protein called fibrin. If a clot is not treated, it could travel to the brain and cause a stroke, or travel to the lung and block a main artery (known as a pulmonary embolism). Anticoagulants help to prevent such harmful blood clots from forming.
They are most commonly prescribed for people who have an abnormal heart rhythm, such as atrial fibrillation, or for those who have an artificial heart valve. Both of these conditions increase the risk of a blood clot forming inside the heart, which can then increase the risk of having a stroke.
Anticoagulants are particularly valuable for treating clots that have already formed, such as those that develop in the veins of the legs (deep vein thrombosis).
Whilst taking an oral anticoagulant it is important to carry an anticoagulation card with you and inform any health care professionals, of your treatment.
You will only be prescribed one of the following: Warfarin or a Direct Oral Anticoagulant (DOAC).
Warfarin
Warfarin has been prescribed as an anti-coagulant for many years. It acts on vitamin K, an essential factor for the formation of various clotting factors in the body.
Warfarin can be prescribed to prevent clots forming for a number of different reasons. You may be prescribed warfarin if you have an abnormal heart rhythm, if you have a certain type of artificial heart valve or if you have had a clot in the leg or lungs.
There is no standard dose for Warfarin. The dose is guided by your blood clotting time, which is known as your "INR" (International Normalised Ratio). The only way of knowing the correct dose of warfarin for someone is to measure the INR regularly. Once the correct level is found these blood tests will become less frequent.
The main risk with warfarin is bleeding. Usually this is a minor problem but if you are worried about any bruising, observe dark stools, blood in the urine or unusual bleeding, speak to your doctor immediately.
Always tell any health professional that you are taking Warfarin. Warfarin interacts with other medications so if you start or stop other medications you may need to have a blood test to ensure that your INR stays within the desired range.
Interactions with food:
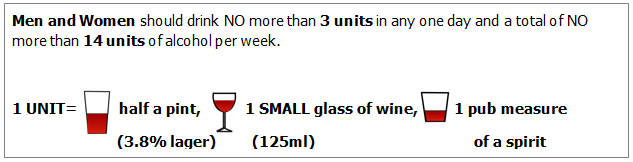
Some foods can also affect Warfarin. The most noticeable one is cranberry juice, which should be avoided as it can increase the effect of the warfarin. Dark-leaved greens can be eaten in small portions, as large amounts taken infrequently can alter the INR. Alcohol can also affect your INR. It is recommended that if you drink alcohol, to drink the same small amount every day. i.e. 1-2 units a day for men and women (see page 61).
If you are taking Warfarin and require further advice about it, then please speak to your anticoagulation clinic or your community pharmacy.
Direct Oral Anticoagulants (DOACs) - Dabigatran, Apixaban, Edoxaban and Rivaroxaban
These anticoagulant medicines have been approved for use for people who have atrial fibrillation, to reduce the risk of having a stroke, for treatment of deep vein thrombosis (DVT) or pulmonary embolism (PE). You cannot take them if you have a heart valve problem or if you have had heart valve surgery.
The main benefit of these anticoagulant medicines is that you don't need to have the regular blood tests that you would need if you were taking warfarin.
These medicines are not affected by the amount of vitamin K in your diet. This means that vitamin K will not reverse the effects of any bleeding that may occur. If there is any bleeding, your doctor will tell you to stop taking the medicine, in order to reduce the level of the medicine in your blood.
These medicines may affect the way that other medicines you are taking work. Your doctor should discuss this with you. It is important that your doctor discusses with you the risks and benefits of taking any of these medicines rather than warfarin.
Dabigatran
Dabigatran helps to reduce the risk of blood clots forming by thinning the blood. It does this by working on an enzyme called thrombin. Dabigatran needs to be taken twice a day as its effects wear off quickly. This means that missing a dose increases the risk of having a stroke. There is an antidote (Praxbind) that can reverse the effect of Dabigatran, if needed in an emergency.
Rivaroxaban and Edoxaban
Rivaroxaban and edoxaban cause your blood to become thinner by affecting the blood clotting process. They need to be taken once a day. It is very important not to miss a dose.
Apixaban
This works in a similar way to Rivaroxaban and Edoxaban, but it should be taken twice a day as its effects will quickly wear off. This means that missing a dose increases the risk of having a stroke.
Side effects of anticoagulants
The main side effect of taking any anticoagulant medicine is bleeding. This happens because the anticoagulant affects the blood-clotting process, helping to prevent blood clots from forming. The anticoagulant may cause internal bleeding, or make bleeding from a minor injury worse.
Any of the following symptoms could mean that your dose of anticoagulant may need to be checked.
- Cuts which bleed for longer than usual.
- Bleeding that does not stop by itself.
- Nose bleeds that last for more than a few minutes. (If a nose bleed lasts for more than 20 minutes, you must go to your GP surgery or to the accident and emergency department of a hospital.)
- Bleeding gums.
- Severe bruising.
- Red or dark-brown urine.
- Red or black bowel movements.
- For women, heavier bleeding during periods, or other vaginal bleeding that is not caused by periods.
If you receive a hard blow to the head or to another part of the body, you should seek medical help without delay to make sure you don't have internal bleeding as this may not be noticeable straight away. If you are worried, contact your GP or anticoagulant clinic, or go to the accident and emergency department at your local hospital. Take with you your anticoagulation treatment booklet and any other medicines you are currently taking.
If you are taking an oral anticoagulant and require further advice about it, then please speak to your anticoagulation clinic or your community pharmacist.
Amiodarone
Amiodarone is used to treat an irregular heart rhythm; it works by correcting this rhythm and slowing the heart rate if it is beating too fast. It is usual to start taking amiodarone three times a day, reducing to twice a day after 7 days, then once a day after a further 7 days. It is then continued once a day.
Side effects associated with amiodarone include:
- Feeling sick
- Blurred vision, it is recommended to have an eyesight test each year as you may develop deposits in the eyes. These should not affect your vision but you may find that you are dazzled by car headlights if you drive at night.
- Feeling either extremely tired and weak, or extremely restless and agitated; either of these can be caused by changes in thyroid function. It is important to have you thyroid function checked every 6 months.
- Blue or grey marks on areas of skin exposed to the sun due to increased sensitivity to the sun. It is advisable to use a high factor sunscreen (at least factor 15, that protects against UVA and UVB) to protect any exposed areas of skin whilst taking amiodarone.
- Changes in the way things taste, feeling shaky, nightmares and difficulty sleeping.
If you are experiencing any of these side effects and they persist or become troublesome speak to your doctor or pharmacist.
Amiodarone can stay in the body for a number of weeks after taking the last dose, so side effects may continue even after stopping the drug.
If you experience any of the following rare but possibly serious symptoms contact your doctor for advice straightaway:
- Breathing difficulties or unexplained cough.
- Yellowing of skin or whites of your eyes that could be a sign of jaundice.
- A severe skin rash that could be a sign of an allergic reaction
Other medications can interact with amiodarone so always check with a pharmacist when buying medicines that they are safe to take together. Grapefruit juice can increase the level of the drug in the body so it is best to avoid this whilst taking amiodarone.
Buying Medicines online, or from health food shops
These sources may not be reliable in terms of the drug's content. Generally it is not safe to buy from sites unless they are registered with the Royal Pharmaceutical Society of Great Britain and displaying this logo.

If you use herbal remedies or supplements, it is wise to check with your pharmacist that there is no interaction between these and your prescribed medication.
Paying prescription charges
If you pay for your prescriptions a pre-payment prescription certificate(PPC) may help with the cost. If you need more than 13 prescribed medicines each year, you could save money with a 12-month PPC. You can also buy a three-month PPC, which will save you money if you need more than three prescribed medicines in three months.
To buy a PPC go to: https://apps.nhsbsa.nhs.uk/ppcwebsales/
Or for telephone assistance call: 0300 330 1341.
Cardiac Rehabilitation
Advice and Education - How can I reduce my risk of further Coronary Artery Disease?
For the majority of patients, there are strong reasons why Coronary Artery Disease has occurred. These reasons are called 'risk factors' and relate to lifestyle and health. A 'risk factor' is something that increases people's risk of getting coronary artery disease. There are several known addressable risk factors for coronary artery disease. The main ones are:
Otherwise known as Hypertension; this refers to a higher than normal pressure flowing through the arteries of the body. As well as affecting the coronary arteries, it may lead to damage to kidneys, brain, eyes and other organs in the body. If you are known to have high blood pressure, you are likely to require antihypertensive medication to control it. It is not uncommon to require more than one medication, sometimes up to four. It is important this medication is taken regularly as prescribed, and must not be stopped suddenly unless under medical supervision. Your GP may ask you to occasionally monitor your own blood pressure at home. As previously stated eating a low salt/sodium diet will help with high blood pressure.
For more information visit the British Hypertension Society, www.bhs.org.uk.
Diabetes is a condition in which the blood sugar is raised to an extent that it leads to damage of the blood vessels throughout the body. Patients with diabetes are at a higher risk of heart attacks. If the blood sugar is only slightly elevated, you may not be aware that you are affected. Blood sugars are routinely checked after a heart attack and if persistently raised, you will require regular treatment.
If you are diabetic, it is important to gain good control of your blood sugar. This reduces the chance of a narrowing developing in the heart's arteries. All patients diagnosed with, or a suspected diagnosis of, diabetes should have regular reviews of their diabetes with their Practice nurse, GP or with the Diabetic Team at the hospital.
pre-Diabetes
Healthy Eating in Diabetes
Many of us do not take enough exercise. It is important to review just how active you used to be. Some forms of exercise are harmful, particularly those that are associated with sudden extremes of effort or require a lot of straining. e.g. heavy weight lifting. The best exercises involve a lot of free movement, with little resistance i.e. cardiovascular exercise. These include walking, jogging, cycling and swimming.
Physical activity helps:
- Lower high blood pressure and prevent high blood pressure from developing.
- Improve your blood cholesterol levels.
- Maintain, or reach, a healthy weight.
- Control your diabetes, if you are diabetic.
- Improve general well being, and speed up recovery following a heart attack.
Once you have completed a cardiac rehabilitation programme, aim to exercise 5 times a week for at least 30 minutes, at moderate intensity (i.e. an exercise that makes you feel warm and slightly out of breath). Along side this, keep as physically active as possible e.g. housework, gardening, hobbies, golf, bowling. In general be more active more often.
For advice on how to gain the most benefit from exercise, speak to the Cardiac Rehabilitation Team.
Too much alcohol can damage the heart muscle, increase blood pressure and also lead to weight gain. During the weeks after your heart attack or heart surgery it is best to limit the amount of alcohol you drink. Small amounts, for example a half pint of beer or a glass of wine a day, will do you no harm. If you are taking sleeping tablets, remember that alcohol will have a more powerful effect.
If you have heart failure, it is recommended you limit alcohol as much as possible because of the damage it causes to the heart muscle. Should you have heart failure caused by alcohol you should avoid alcohol completely; abstaining may even reverse some of the damage to the heart muscle.
Everyone should avoid binge-drinking but this is particularly important if you are taking anticoagulant tablets (i.e. warfarin). Too much alcohol can interfere with the anticoagulation process so, if you do drink alcohol, it is better to have a small amount on a regular basis.
Remember to drink responsibly, visit: www.drinkaware.co.uk
Top tips for drinking Alcohol sensibly

If you were/are a smoker, you will have been strongly advised, whilst in hospital, that you MUST stop smoking. Although easy to enforce in hospital, once home, it may be tempting to slip back into your old habits. If you continue to smoke after having had a heart attack, you double your chances of having another one compared to if you stopped.
Although it's not something that's going to be easy, this is one of the most important lifestyle changes you can make. Speak to your practice nurse, GP or local Smokestop team for more advice and help regarding quitting and which aids are available to you (e.g. nicotine patches/gum).
Bournemouth and Poole Smokestop is part of the NHS and provides FREE support and advice to assist people wishing to give up smoking. Specially trained staff can help you to understand why you smoke and give you ways to cope when you decide to stop. Tel: 0300 30 38 038
NHS Smoking Helpline Tel: 0800 1690169
Or visit: www.nhs.uk/smokefree
The impact of smoking

Stressors are a part of everyday life. There is some evidence that those who find it difficult to manage their stressors are more likely to suffer from heart attacks. Stress puts an immediate strain on the heart by increasing blood pressure and the pulse rate. Relaxation and meditation may help you to avoid this. For more information and advice on stress and your health visit: www.nhs.uk/Conditions/stress-anxiety-depression.
Breathing relaxation exercise.
This calming breathing technique for stress, anxiety and panic takes just a few minutes and can be done anywhere.
You will get the most benefit if you do it regularly, as part of your daily routine.
You can do it standing up, sitting in a chair that supports your back, or lying on a bed or yoga mat on the floor.
Make yourself as comfortable as you can. If you can, loosen any clothes that restrict your breathing.
If you're lying down, place your arms a little bit away from your sides, with the palms up. Let your legs be straight, or bend your knees so your feet are flat on the floor.
If you're sitting, place your arms on the chair arms.
If you're sitting or standing, place both feet flat on the ground. Whatever position you're in, place your feet roughly hip-width apart.
- Let your breath flow as deep down into your belly as is comfortable, without forcing it.
- Try breathing in through your nose and out through your mouth.
- Breathe in gently and regularly. Some people find it helpful to count steadily from 1 to 5. You may not be able to reach 5 at first.
- Then, without pausing or holding your breath, let it flow out gently, counting from 1 to 5 again, if you find this helpful.
- Keep doing this for 3 to 5 minutes.
If you would like to speak to someone and live in Dorset you can self-refer to steps2wellbeing visit: https://www.steps2wellbeing.co.uk/

Everyone benefits from eating a healthy, balanced diet. Concentrating on certain aspects of the diet can help prevent further narrowing in the heart's arteries from developing. A Mediterranean style diet is a healthy diet that is generally low in fat (particularly low in saturated fat), low in salt, high in fibre (roughage). This can be achieved by eating more wholegrain bread, pasta, fruit, vegetables and fish; less red meat; and replace butter and cheese with products based on plant oils. Research has shown, that following a Mediterranean style diet can reduce the chance of developing conditions such as heart disease, type 2 diabetes, high blood pressure, obesity and even Alzheimer's disease. The following chart is a guide on how to follow a Mediterranean style diet.
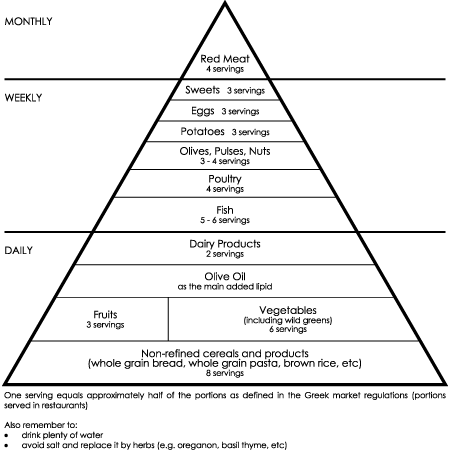
Supreme Scientific Health Council 1999
Fruit & Vegetables
Eating plenty of fresh fruit and vegetables not only helps to prevent constipation, by increasing fibre intake; but also provides the majority of the vitamins and minerals required by the body. Current recommendations are to eat 5 (to 9) portions of fruit and vegetables in a day. Typically a portion is a handful of fruit/vegetables. A glass of fruit juice is considered a portion, but potatoes do not count as part of the 5 (to 9) portions. Aim to eat fruit and vegetables of different colours, such as red peppers, green apples, yellow melon etc... This will enable you to obtain a variety of vitamins and minerals from your food.

Salt
No more than 6g/1 level teaspoon of salt per day. People who have a lot of salt in their diet are more likely to have high blood pressure. To cut down on your salt intake, initially try not to add salt to your food at the table. Later on, also try cooking without adding any salt (use herbs and spices to add flavour instead). You may want to check the ingredients' labels on food packaging, to find out how much sodium the food contains. You will find that within about a month your taste buds will have adjusted and you may not like salty foods. You will get all the salt you need from the 'hidden salt' in processed foods and bread.
Cholesterol & Fats
Cholesterol is a fatty substance made mainly in the liver, which circulates in the blood and contributes to the gradual narrowing of the coronary arteries (atherosclerosis). To help reduce your cholesterol level you need to do the following:
- Cut right down on saturated fats (e.g. butter and fats from animal origin). Try using monounsaturated and polyunsaturated fats. e.g. olive oil/ sunflower oil (including spreads). Remember all fats contain calories. Swapping to a lower saturated fat will not, however, reduce the calories.
- Reduce the total amount of fat you eat - especially if you are overweight. For example, you could eat less pastries, crisps or biscuits, and replace them with healthier alternatives such as fruit. Or, at mealtimes, you may be able to cut down on the amount of fatty foods by filling up with starchy foods such as bread, pasta or rice instead.
- Eat lots of foods high in fibre. This helps your body to reduce absorption of fats. Eat 5-9 portions of fruit or vegetables a day, as these contain high levels of fibre.
Examples of changes to diet:
- Change from full fat to semi-skimmed or skimmed milk
- Use half fat cheese (or a smaller portion of full-fat cheese)
- Use skimmed milk for cooking
- Eat fewer cakes and biscuits
- Swap red meat for white meat, e.g. beef/pork for chicken/fish
- Choose leaner cuts of meat, remove the skin from chicken.
- Grill rather than fry foods
- Dry roast meat
- Cut visible fat off meat
Treats are OK e.g. fish and chips, cream tea, and birthday cake, but only occasionally.
For more information on healthy eating visit: www.nhs.uk/live-well/eat-well.
Lose Weight
If you are overweight, reducing your weight will reduce the workload of your heart, help keep your blood pressure down and lower your cholesterol. Weight gain is directly related to the calories you consume. Remember that losing weight involves both eating healthily (by reducing the amount of fat in your diet and reducing your calorie intake) and by increasing your daily physical activity.
Cardiac Rehabilitation
Advice and Education - Heart Conditions and Treatment
What is a Percutaneous Coronary Intervention (PCI) or Angioplasty?
Percutaneous Coronary Intervention is a procedure that widens a narrowed coronary artery, using specialized catheters. PCI can be performed as a planned procedure or as an emergency for someone who has an acute blockage/narrowing of the coronary arteries, such as a person suffering with severe angina or a heart attack. PCI can also be used if you have had coronary bypass surgery but a coronary graft has become narrowed.
The procedure is very similar to that of an angiogram. The cardiologist uses X-ray screening to guide a balloon mounted on a catheter to the narrowing in the coronary artery. The balloon is then gently inflated so that it compresses the fatty tissue responsible for the narrowing. This widens the artery and to hold the area open, a stent is usually left in place. As the balloon is inflated, angina symptoms may occur, but the pain eases very quickly when the balloon is deflated. A PCI will often take longer than an angiogram.
Prior to having a coronary angioplasty and for a defined period afterwards (which varies), certain 'anti-platelet drugs' will be prescribed to help both prevention of future coronary events and stent blockages.
If you have a stent and there is any question of the Clopidogrel/ Ticagrelor/Prasugrel being stopped by anyone, it must firstly be confirmed with your Cardiologist (Consultant at the hospital).
Sometimes, if the person has agreed to it beforehand, and the circumstances are right, the doctors may perform the PCI at the same time as the coronary angiogram.
Technical advances in PCI have led to the use of tools such as a laser or Rotablator (miniature diamond drill) and special balloon-only procedures. These can assist the interventionist in opening up an artery. However if PCI cannot be performed, or has been unsuccessful, the cardiologist may recommend a Coronary Artery Bypass Graft.
What is Rotablation?
What is Coronary Artery Bypass Grafting?
Coronary Artery Bypass Grafting is an operation where a blood vessel (an artery or vein) is removed from one part of the body and attached on to the heart’s coronary arteries to 'bypass' a blocked coronary artery.Several of these 'bypass' grafts may be needed and at least one of the donor blood vessels used as a graft will usually be an artery. The donor blood vessels used may be obtained from the inside of the chest wall, the leg or the arm.
Patients needing cardiac surgery will be referred to a cardiac surgeon at a specialist cardiac surgical centre, (for example, Southampton General Hospital).
Patients are usually admitted to the centre the day or the day before their operation. The length of stay varies, but is usually 4-7 nights following the surgery. In the initial 24-48 hours, following the surgery, patients require close monitoring in an Intensive Care or High Dependency Unit.
If you require Cardiac Surgery and are waiting in hospital for transfer, the ward staff and Cardiac Referrals Co-ordinator will be organising your transfer to the specialist cardiac centre. If you are waiting at home for the surgery, the Cardiac Referrals Co-ordinator will be assisting with your referral for Cardiac Surgery.
Cardiac Surgical Referrals Co-ordinator 01202 704404
What is Valve Disease?
The pumping action of the heart is assisted by four valves that control the flow of blood in one direction through the chambers of the heart. They are composed of thin tissue and despite being in constant use, are remarkably durable. On each side of the heart the valves form the only structural link between the chambers.
A valve can fail in two ways. The valve can leak (termed 'incompetence' or 'regurgitation') or narrow (called a 'stenosis'). Often a valve can be both leaking and narrowed. The following situations illustrate what may happen.
The first is a narrowing (stenosis) of one of the two valves on the left side of the heart. Narrowing of the Mitral Valve, nearly always a consequence of rheumatic fever as a child, produces damming up of blood within the left atrium which in turn causes fluid accumulation in the lungs. The consequence of this is shortness of breath. The heart's pacemaker is often upset and irregular fast rhythms are common in patients with advanced mitral stenosis. Narrowing of the other left heart valve, the Aortic Valve, means that not enough blood can be circulated to the body. This is especially noticeable during times of effort and patients frequently present with dizziness.
The second situation is one where a valve is leaking. Again, this is more common and more likely to be of importance when this involves the left side of the heart. Additional strain is put on the pumping chambers because for every heartbeat a variable proportion of blood is going in the wrong direction and has to be emptied out each time to try and maintain a normal circulation. The usual symptom of an overtaxed heart, in this situation, is breathlessness. If the right side of the heart is involved then fluid collects in the ankles or abdomen rather than the lungs.
Prevention of Infection
Before discussing those patients requiring some intervention, it is important to mention preventative measures. Anyone with Valvular Heart Disease runs a slight risk of infection of the valve. Whenever bacteria or other organisms get into the blood stream the body's defences rise up and kill these organisms. If however, the bacteria can hide away in a diseased valve or other abnormal lining structure of the circulation, then they can remain undisturbed and immune to one's natural defences. The organisms can then multiply and infect the heart leading to serious structural damage.
A small dose of bacteria invading the blood is of no consequence but during certain procedures such as dental work near the gums, some surgical procedures or an investigation of one of the passages, the amount of bacteria entering the blood can be considerable. In this situation there is a small risk of infection of the heart lining (called endocarditis). Such a risk can, in the case of dentistry, be reduced by good oral hygiene. It is important that you visit your dentist six monthly and take good care of your teeth and gums. In some circumstances your cardiologist may advise antibiotics before a dental procedure as a precaution.
Treatment
Those patients who develop symptoms related to their valvular insufficiency will require some form of treatment. In the majority of cases this is medical. Tablets used are to reduce fluid accumulation (diuretics) and to open up the circulation and prevent backward flow (vasodilators). Other drugs may be used to correct the heart rhythm if this has been disturbed. Patients with turbulent blood flow, particularly if linked to a persistently irregular heart rhythm, may need to go onto a blood thinning treatment to prevent clot formation. Such treatment can be life-long.
In a small proportion of patients, a surgical solution is necessary. This usually means an operation on a heart valve. Diseased valves can sometimes be repaired but more commonly require replacement.
Repair
The form of repair depends on which valve is involved and the type and severity of the abnormality. For example, a leaky mitral valve can sometimes be repaired. Valve replacement is however more common (and is the norm for the aortic valve).
Replacement
There are two main types of artificial heart valve. The first are artificial man-made valves (prosthetic/mechanical) and the second type are constructed from human or specially treated animal tissues (biological/bio-prosthetic valves). Each have their own attributes and both give excellent results. The decision as to which type to use depends on many factors. The surgeon may not be able to make a decision until the time of the operation. The main concern for the patient is that the prosthetic valves tend to last longer but require the indefinite use of a blood thinning drug (anticoagulant). Most patients who require a heart operation find their previous symptoms improve or disappear. Some drug treatment is reduced or withdrawn completely and for those, who prior to the operation were not able to work because of their symptoms, are often well enough to return to their previous occupation.
What is Atrial Fibrillation?
What is Heart Failure?
The term 'heart failure' is used when the heart muscle is impaired and failing to deliver as much blood and oxygen as the body requires. This can lead to breathlessness, tiredness and swollen ankles.
This may happen for a number of reasons, including, weakness or stiffness of the heart muscle, narrowed or leaking valves and abnormal heart rhythms. The most common causes of heart failure are heart attacks, high blood pressure and cardiomyopathy (a disease of the heart muscle). It may also be caused by, valve disease, congenital heart disease, uncontrolled irregular heart rhythms, alcohol and recreational drugs, and some chemotherapy.
Your consultant will tell you if you have heart failure, and may refer you to a Heart Failure Nurse specialist, who will contact you to offer support.
The British Heart Foundation produce a detailed booklet called "An everyday guide to living with Heart Failure". This can be found under their publication section at www.bhf.org.uk
Treatment for heart failure aims to control symptoms and manage the causes of heart failure. With the support of a heart failure nurse you will be shown what you can do to help you manage your heart failure. This includes, taking your medication, monitoring your weight and changes in your symptoms, eating healthily, reducing salt intake, controlling your fluid intake, limiting alcohol, stopping smoking and keeping active.
If you have heart failure, it is important to keep an eye on your weight. This is because, if your weight goes up, it may be that too much fluid is building up in your body. Weigh yourself every morning and tell your doctor or Heart Failure Nurse about any sudden weight change (for example, if your weight goes up by about 4 pounds – just under 2 kilograms – over two days), or if you start getting more breathless, or have more ankle swelling. It may be that a slight change in your medication (such as water tablets) can improve the symptoms you have.
Bournemouth Heart Failure Team: 01202 726079
Visit: www.cardiomyopathy.org / www.bhf.org.uk









