RANV/SDEC Clinic
New content coming soon
Hi STEPS
Stroke Exercise and Education Group

HI STEPS is a rolling 12 week exercise and education programme for people following a stroke. The programme is particularly targeted at people with milder stroke symptoms who are discharged without on-going therapy input.
HI STEPS aims to build people's knowledge to manage their health and wellbeing following a stroke, their confidence to exercise and to make and sustain positive behaviour changes.

Referral criteria:
- Recent stroke symptoms, treated under the care of the UHD Stroke team
- Discharged home without therapy input
- Would be suitable for group exercise (could be independent using gym equipment/light touch support)
- Is happy/consents to participate in HI STEPS group
- Is able to independently attend Christchurch Day Hospital every Monday for 12 weeks (no hospital transport available)

Timings and Structure:
- HI STEPS runs every Monday (not bank holidays) from 12:40-14:45.
- On arrival attendees split into 2 groups each having 1 hours gym based exercise and 1 hour of education
- New participants will be asked to attend their first session early to allow 1:1 assessment with a physiotherapist before the group starts.
Meet the HI STEPS team:
HI STEPS is run by a small group of staff including:
- Lauren Higgs and Rebecca Marsh (Physiotherapists, Christchurch Day Hospital)
- Grace Jareno (Exercise Instructor, Christchurch Day Hospital)
- Stephanie Heath (Stroke Follow up Practitioner)
- Irma Konovalova (Clinical Psychologist, Stroke ESD Team)


Educational Topics included in the programme:
- What is stroke?
- Managing blood pressure?
- Benefits of exercise?
- Managing energy and fatigue
- The emotional impact of stroke
- Cholesterol management
- Doing what matters to me
- Community based support (with external guests from Help & Care, BH Live Exercise referral scheme, Live Well Dorset)
- The Stroke Association – who we are and what we do (with the East Dorset Stroke Association Support Workers)

What participants told us they got from their HI STEPS experience? (Feedback from previous HI STEPS participants)
- “Inspiration and focused knowledge”
- “The whole programme has helped, to go straight into it following my stroke gave me information and self-help tips I wouldn't have known, mentally it helped just knowing that help is at hand”.
- “Information/confidence to move forward. Ability to change my life the correct way.”
- “Improved confidence, education about statins”
- “Increased strength and a visible improvement by recording exercises done. Increased my knowledge on stroke related topics”

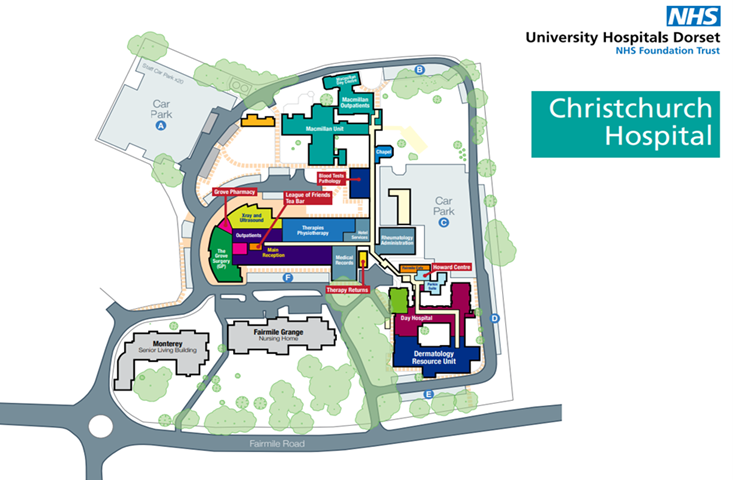
How to find us:
If you are attending the HI STEPS Group at Christchurch Hospital for the first time, once on the hospital site, follow the signs for the Day Hospital and park in Car Park C. Enter the building via the Day hospital entrance and check in at the reception desk. A parking permit will be provided for you for the duration of the programme.

HI STEPS Resources:

 back to welcome
back to welcome
Early Supported Discharge Team (ESD)

The UHD Stroke and Neuro Early Supported Discharge Team (ESD) provides early, intensive specialist rehabilitation for stroke and neurological patients for up to six weeks based on clinical need.

The team helps patients to leave hospital and return to their own homes so they can maximise independence as quickly as possible after their stroke or neurological event. Rehabilitation is centred around their individual goals and delivered in a setting that is meaningful to their lives.
Patients are referred directly from the stroke unit or hospital wards and are usually seen within a few days of discharge.
The service is made up of stroke/neuro specialist staff that covers a 7 day a week service to provide specialist rehabilitation.

The ESD team includes:
- Physiotherapists
- Occupational Therapists
- Nurses
- Speech and Language Therapists
- Clinical Psychology
- Rehabilitation Assistants
- Consultant Therapist for Stroke and Neuro


Rehabilitation goals will depend on the individual but tasks may include:
- Mobility and balance
- Washing and dressing
- Kitchen tasks
- Shopping
- Memory strategies
- Talking
- Swallowing
- Emotional support
- Care givers support, teaching and education
- Lifestyle and health

After a period of ESD rehabilitation in their own home patients can be referred to the appropriate community services for on-going rehabilitation if required.
In addition to ESD some patients may also be supported by a care package or a community rehabilitation team. We work closely with these teams to update them on the patients' progress and what goals they can continue to work on.
Catchment area
ESD covers Bournemouth (BH1-BH11), Poole (BH12-BH18), and parts of Dorset (BH21, BH22, BH23, BH31 and parts of BH24). The patient needs to be registered with a Dorset GP.
Contact details
To contact the team for more information:
Tel: 0300 019 4473
General enquiries and to discuss a referral: This email address is being protected from spambots. You need JavaScript enabled to view it.
Team lead: This email address is being protected from spambots. You need JavaScript enabled to view it.
Consultant Therapist (Stroke/Neuro): This email address is being protected from spambots. You need JavaScript enabled to view it.
HI-REPS
(HI-REPS – High Intensity Repetitive Exercise Program for Stroke)

The HI-REPS Arm Group is an intensive arm exercise programme for people following a stroke. The programme is for people with moderate arm deficits. It requires a referral by one of our UHD or Dorset HealthCare Neuro Therapy Teams.
Speech and Language Therapy
Speech and Language Therapists work with people with speech and swallowing difficulties.
Speech and Language Therapists are an integral part of the Stroke Unit multi disciplinary team at Bournemouth Hospital. They usually wear a white tunic with yellow or pink trim and black trousers. They work across the Stroke pathway including the Hyperacute service, rehabilitation pathways and into the Early Supported Discharge team or Community Rehab teams, which can be involved when patients first go home.
Swallowing
On admission to the stroke unit, our specialist nurses will complete a water swallow screen. If this identifies you at risk of swallowing difficulties then you will be automatically referred to the speech and language therapists. They will do a more in depth assessment and advise you of any strategies that can help your swallow. They may recommend you modify your diet to make it easier to chew or thicken your drinks. This will be discussed with you during the assessment.
Some patients may require an instrumental assessment of their swallow (videofluoroscopy). This is a moving xray where you will be asked to swallow barium and images will be taken of your swallow.
If your swallow is not safe, the medical team may recommend that you have a temporary feeding tube (NG tube). The medical team, dietitian and speech therapists will regularly review to work with you and your family to return to oral intake.
Communication
People with stroke can experience difficulties communicating. This can include understanding what someone is saying and finding the right words. It can also affect reading and writing. If you have communication difficulties when admitted then you will be seen by a Speech and Language Therapist for assessment and advice. If further therapy is needed then your SLT will work with you to decide therapy goals and approaches. This may include 1:1 therapy, providing friends and family with advice and/or group work.
We run a communication group every week. Education around strokes and communication difficulties is provided. It allows people with communication difficulties to build their confidence and practice their strategies in a functional and enjoyable setting.
Our PACT group (People with Aphasia Communicating Together) runs once a month. This is an opportunity for people with aphasia in hospital and people who are now at home to meet and share their experiences. This is facilitated by the SLT team and volunteers who have previously had strokes.