Further information and support

This website contains current and accurate information about diagnosing, treating and living with gynaecological cancer.

Provides help and support for people affected by cancer, including gynaecological cancer.

Includes information about risk factors, symptoms and treatment of cervical cancer and how to access emotional and practical support.

Includes information about symptoms, diagnosis and treatment of ovarian cancer and provides support to women with ovarian cancer.

Includes information about symptoms, diagnosis and treatment of ovarian cancer and provides support to women with ovarian cancer.

Includes information about the risk factors, signs and symptoms, diagnosis and treatment of gynaecological cancers.

Information about services and support for people affected by cancer in Dorset, Hampshire and the Isle of Wight.

Local and national cancer support groups


Transport services

Diet and exercise advice


Fitness Studio exercise videos

BDA - The Association of UK Dietitians
Financial and benefits advice



Mental health support


Bereavement support
Adults

Children and young people

Apperance

Meet the team
Meet the team at University Hospitals Dorset - Bournemouth Hospital
 Lead clinician - Miss Rachana Dwivedi
Lead clinician - Miss Rachana Dwivedi
Miss Dwivedi works alongside the Poole Dorset Cancer Centre. Her role is to manage women who are referred to secondary care for suspected gynaecological cancer. She manages their diagnostic pathway including treatment and follow up. She has dedicated diagnostic clinics (post-menopausal bleeding, colposcopy and gynaecology outpatient department with fast track referrals) . She attends weekly Multi-Disciplinary Meetings and works closely with cancer centres.
 Lead cancer nurse specialist - CNS Mary Brinsdon (Gynaecology Oncology Clinical Nurse Specialist)
Lead cancer nurse specialist - CNS Mary Brinsdon (Gynaecology Oncology Clinical Nurse Specialist)
Mary has been in post for 7 years. She is the CNS responsible for all co-ordination of all care given to women diagnosed with a gynaecological cancer. This involves the patient's treatment pathway, user issues and provision of written information. Mary also runs a monthly nurse led endometrial cancer follow up clinic.
Mary has attended the Advanced Communication Skills course, Psychological, Gynaecological Cancer and Chemotherapy study days. She has completed a Gynaecology cancer module at the Marsden hospital as well.
Consultants working within gynaecology oncology diagnostic & treatment team:
Gynaecology consultants
Rachana Dwivedi
Alex Taylor
Padma Eedeparali
Mangla Dubey
Gynaecology oncologist consultants
Anni Inamaa
Jonathon Lipiatt
Ianis Biliatis
All three oncology consultants are based at Poole Hospital. If you need an operation at Poole hospital your surgeon will be one of these three consultants and you will see one of them prior to your operation. Anni Inamaa is the Gynaecology oncology consultant who does a weekly clinic at the Royal Bournemouth Hospital.
Radiology specialist consultants
Sonya Snape is the named consultant radiologist at RBH. She takes the lead in imaging for all gynaecological cancers and attends the weekly multi-disciplinary team meeting.
Lead histopathologist consultant
Shereen Hayder
Palliative lead consultant
Megan Haworth
 Medical oncologist consultant
Medical oncologist consultant
Dr Joanne Parkinson
Nurse support team
 Senior nurse colposcopist/ cervical screening provider lead
Senior nurse colposcopist/ cervical screening provider lead
Stephanie Freeman
Stephanie is a BSCCP accredited Colposcopist working in the Colposcopy department of the Jigsaw building. Her role as CSPL involves liaising with external Quality Assurance teams to ensure that the cervical screening programme provided by Royal Bournemouth.
 Gynaecology nurse practitioner
Gynaecology nurse practitioner
Georgie Morrissey (who covers when CNS Mary Brinsdon is off)
CNS administrator
Mrs J Foy
 Cancer support worker
Cancer support worker
Suzanne Bannister. Suzanne Bannister is the Gynaecology Cancer Support Worker and her main role is to conduct holistic needs assessments with patients which result in planning, managing or implementing personalised care and support planning elements for people living with cancer.
Gynaecology Cancer
What are gynaecological cancers?
'Gynaecological cancer' refers to the five cancers that start in a woman's reproductive system – womb, ovarian, cervical, vulval and vaginal.
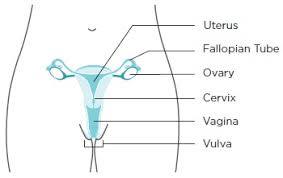
Women's reproductive system
The symptoms, diagnosis and treatment depend on the type of cancer, as outlined in each of the following sections. Further information can be found via the online resources in the 'useful links' section.
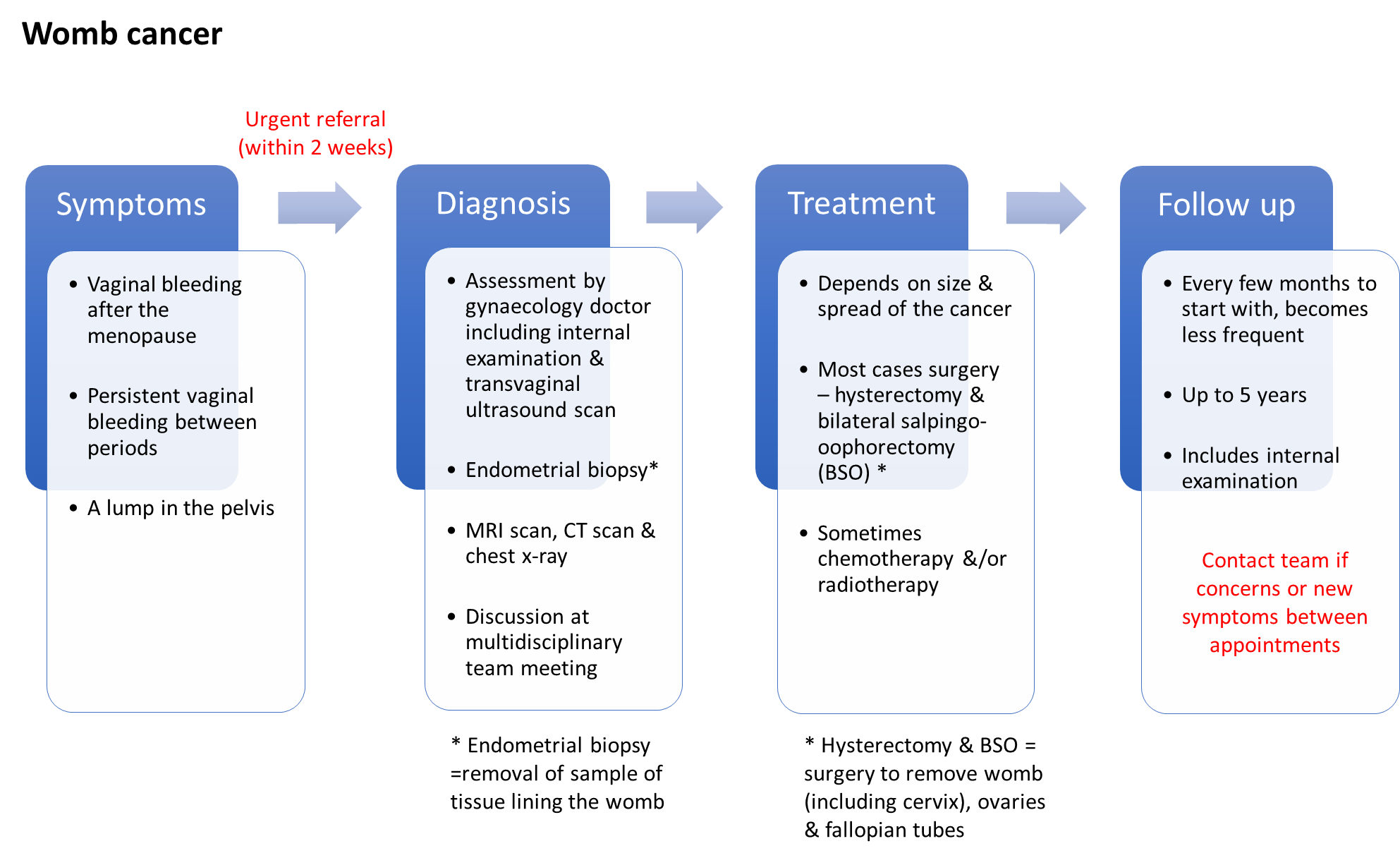
Womb Cancer
Womb cancer is the most common gynaecological cancer with approximately 9,500 new cases in the UK each year. Womb cancer may also be called uterine or endometrial cancer; the endometrium is the lining of the womb where most womb cancers start.
The diagram below illustrates the potential symptoms, investigations used to help diagnose the cancer, possible treatment options and the usual follow up.
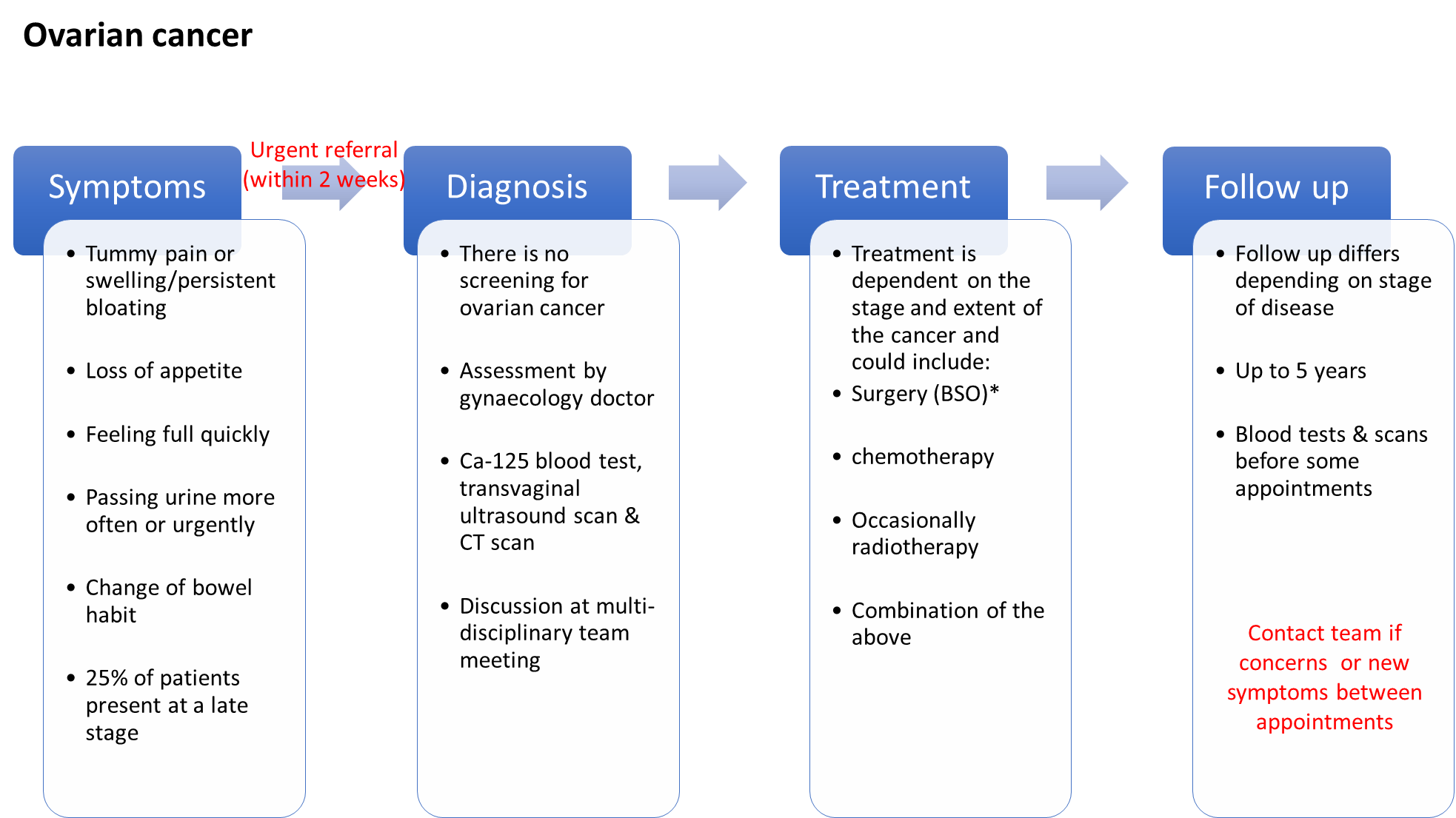
Ovarian Cancer
Ovarian cancer is the second most common gynaecological cancer– around 7,500 women are diagnosed in the UK each year.
The diagram below illustrates the potential symptoms, investigations used to help diagnose the cancer, possible treatment options and the usual follow up.
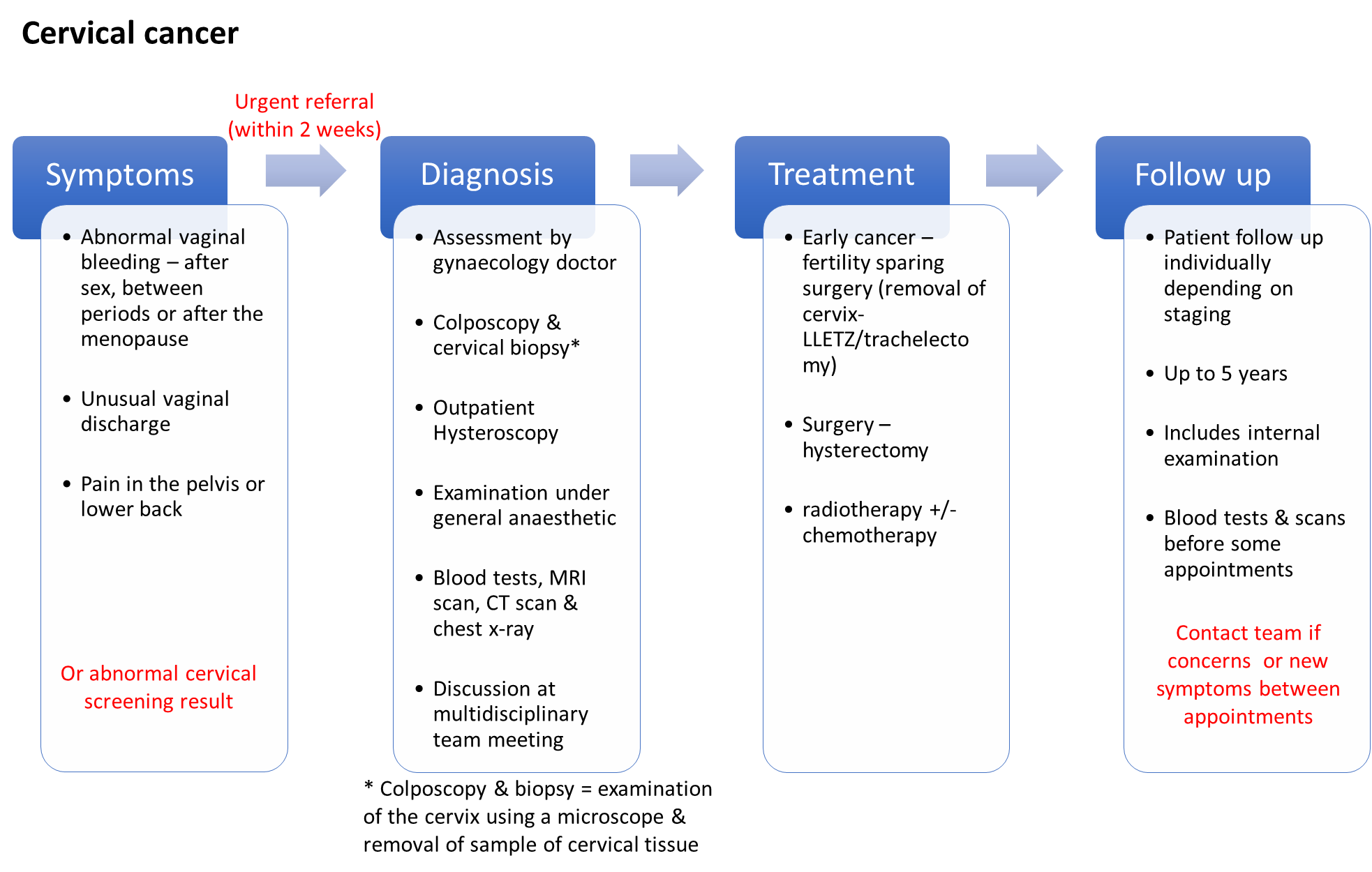
Cervical cancer
Cervical cancer is the third most common gynaecological cancer in the UK - around 3,200 women are diagnosed each year.
It mainly affects sexually active women aged between 30 and 45.
Almost all cases are caused by infection with some types of the human papilloma virus (HPV). It may be possible to reduce your risk by practicing safe sex, attending appointments for cervical screening and stopping smoking. The HPV vaccine, now part of the routine childhood immunisation programme, may also reduce the chance of developing cervical cancer.
The diagram below illustrates the potential symptoms, investigations used to help diagnose the cancer, possible treatment options and the usual follow up.
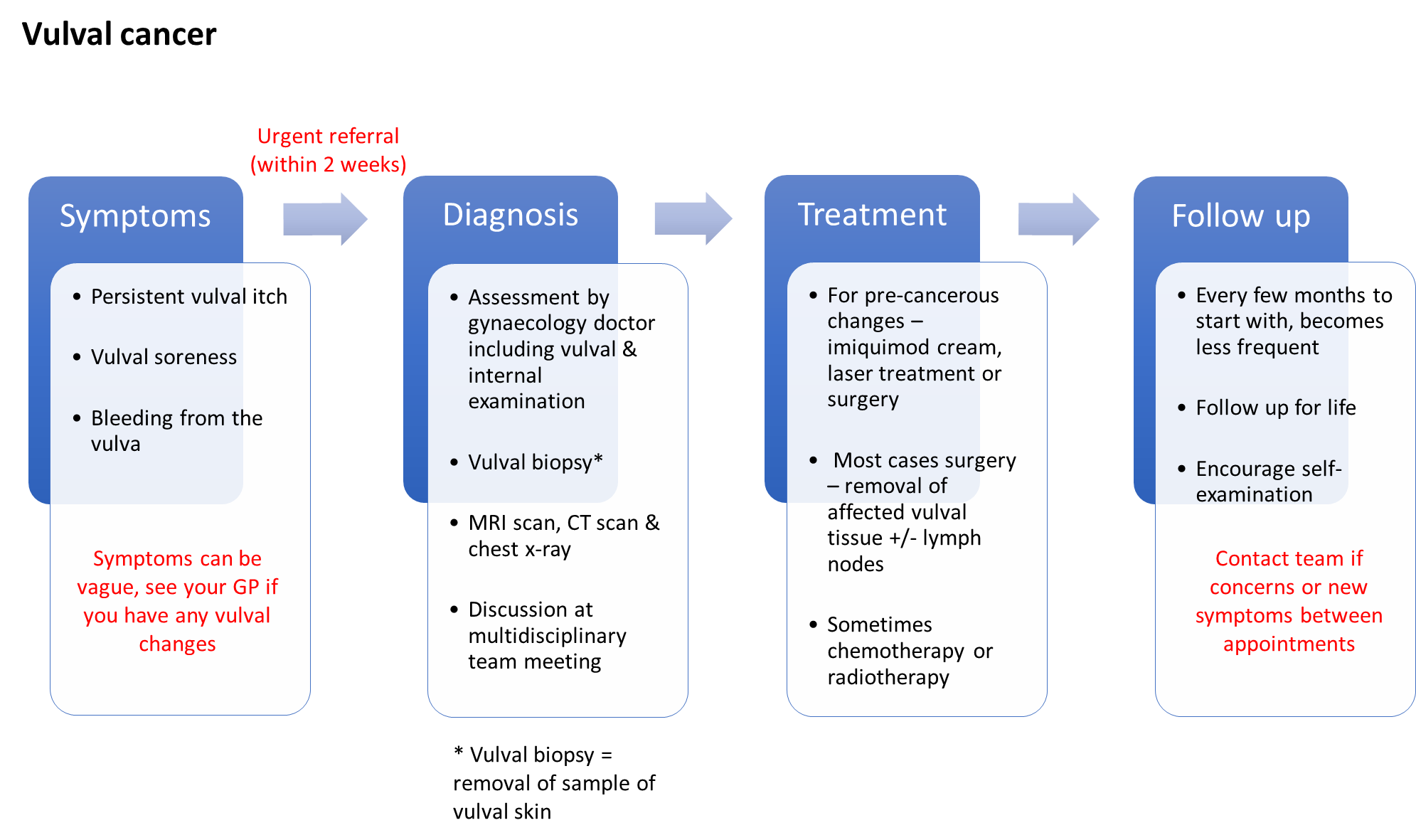
Vulval Cancer
Cancer of the vulva is rare – around 1,300 women are diagnosed in the UK each year. It can start in any part of the female external genitalia (the vulva) but most commonly it affects the inner or outer lips.
Most cases are in women over the age of 65.
Around 50% of vulval cancers are caused by infection with some types of the human papilloma virus (HPV). It may be possible to reduce your risk by practicing safe sex, attending appointments for cervical screening and stopping smoking. The HPV vaccine, now part of the routine childhood immunisation programme, may also reduce the chance of developing vulval cancer.
The diagram below illustrates the potential symptoms, investigations used to help diagnose the cancer, possible treatment options and the usual follow up.
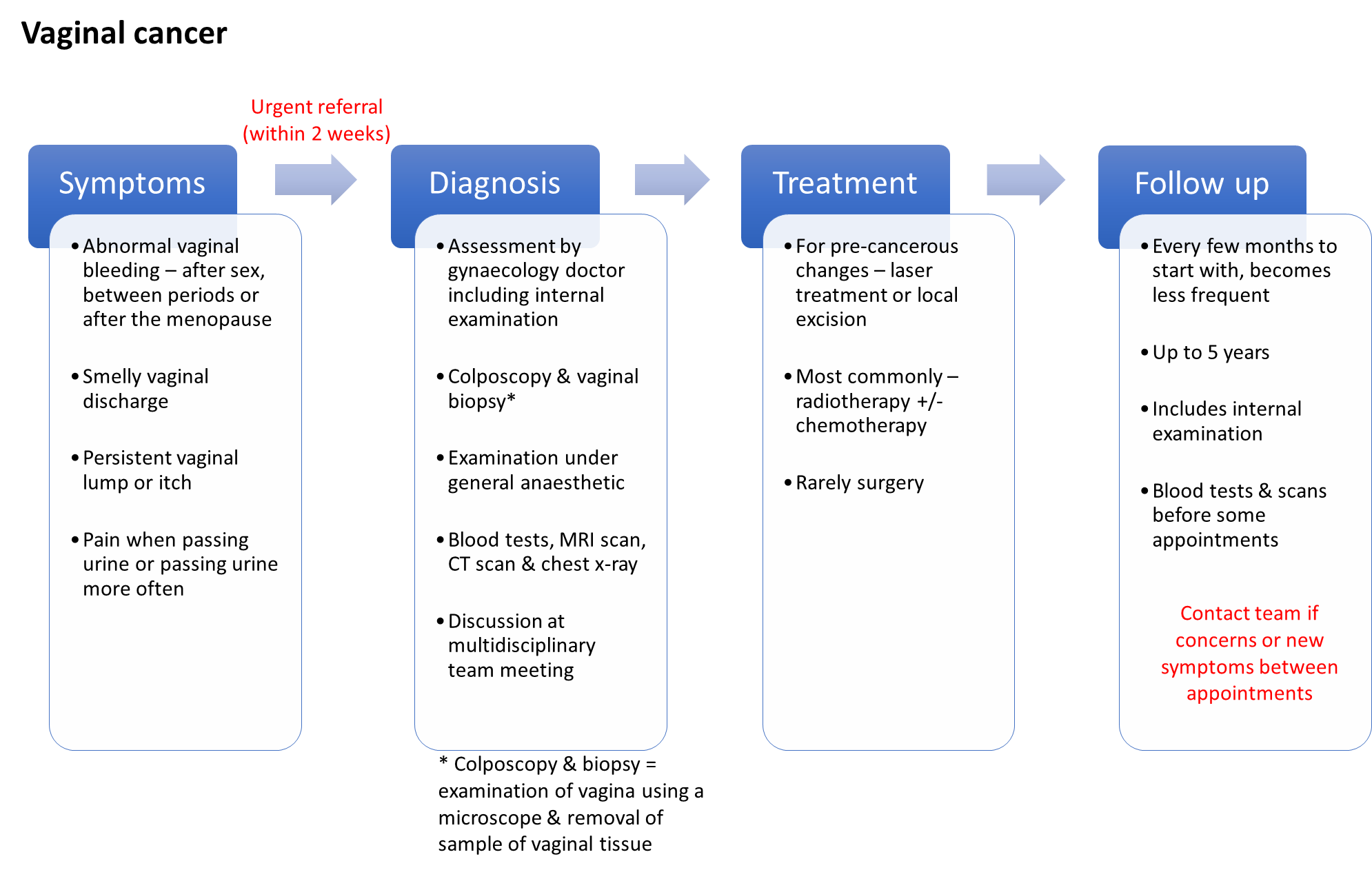
Vaginal Cancer
Vaginal cancers are rare – less than 300 women are diagnosed with this type of cancer in the UK each year. It is more common for cancer to start in an area nearby, such as the cervix or womb, and spread in to the vagina.
Most cases are caused by infection with some types of the human papilloma virus (HPV. It may be possible to reduce your risk by practicing safe sex, attending appointments for cervical screening and stopping smoking. The HPV vaccine, now part of the routine childhood immunisation programme, may also reduce the chance of developing vaginal cancer.
The diagram below illustrates the potential symptoms, investigations used to help diagnose the cancer, possible treatment options and the usual follow up.
Urology Cancer
Remote Follow up for Prostate Cancer Videos
Patient-led follow-up: What is it?
PSA monitoring and surveillance
Signs and symptoms
Hormone therapy
Erectile dysfunction
Physical and emotional effects
Skin Cancer
Information coming soon.









