Patient initiated follow up
This webpage is for people who have been diagnosed with Transient Ischaemic Attack (TIA) and are put onto a Patient Initiated Follow Up Pathway (PIFU).

What is Transient Ischaemic Attack (TIA)?
Transient ischaemic attack or TIA means that someone has experienced stroke symptoms that have quickly resolved. We often use the term ‘TIA’ when people have had stroke symptoms that have lasted less than 24 hours before completely resolving, often the duration of TIA symptoms is even quicker, most people who experienced TIA will have completely resolved within 1 hour of onset of symptoms.
TIA is a medical emergency as it is considered a warning of risk of future stroke symptoms. The risk is greatest in the time immediately following a TIA, it is therefore important that people with TIA symptoms are quickly assessed by specialists. Research has shown that when people with TIA are promptly diagnosed by specialist, investigated with appropriate tests and started on medications risk of early stroke is reduced by as much as 80%.
Resources that will help you understand your diagnosis and common approaches to help reduce risk of further symptoms are available below:
 Stroke Association Transient Ischaemic Attack (TIA) Guide
Stroke Association Transient Ischaemic Attack (TIA) Guide
 Stroke Association Blood Thinning Medications Factsheet
Stroke Association Blood Thinning Medications Factsheet
 Stroke Association Carotid Artery Disease Guide
Stroke Association Carotid Artery Disease Guide
 Stroke Association – How to Reduce your risk of a stroke
Stroke Association – How to Reduce your risk of a stroke

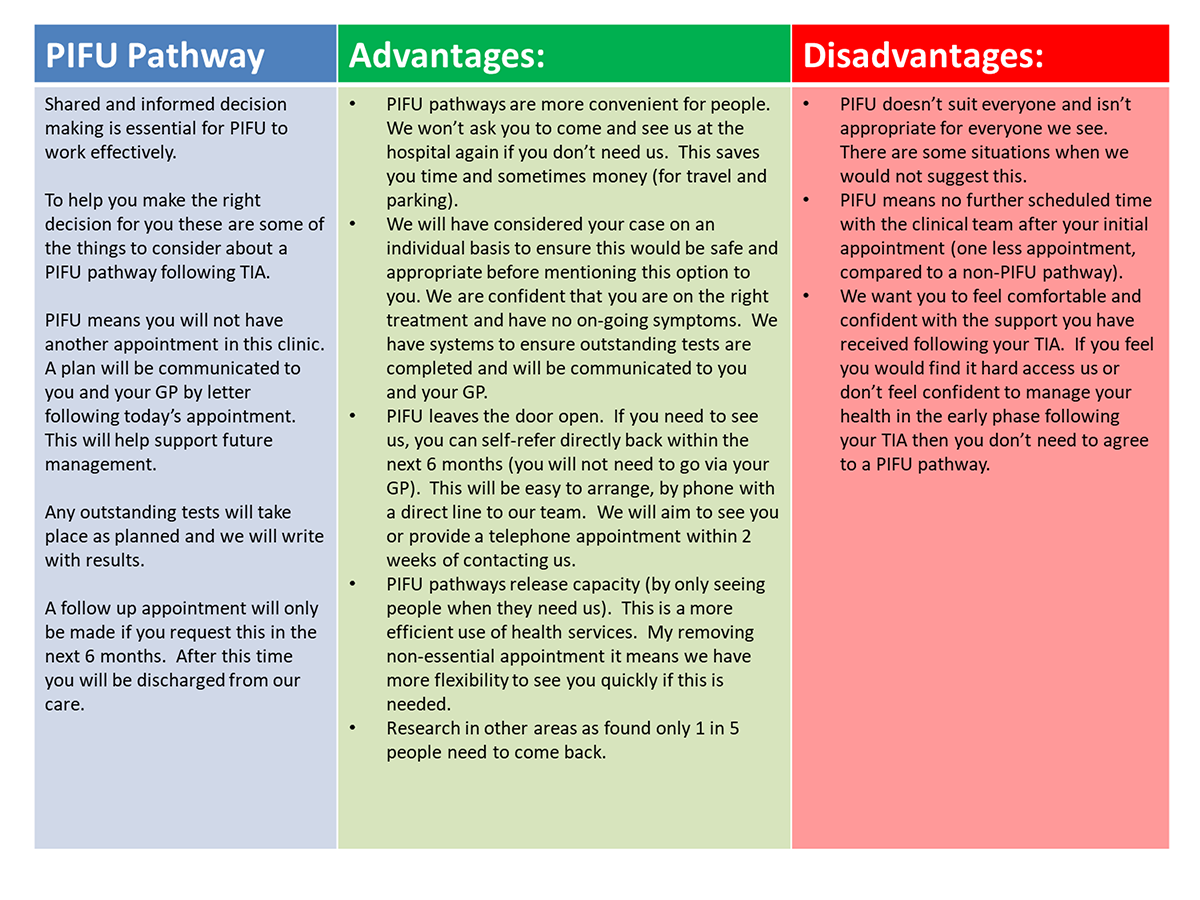
What is Patient Initiated Follow Up (PIFU)?
Patient initiated follow-up or PIFU is a different way of supporting people after the diagnosis of TIA is made. The decision to go on to a PIFU pathway will be made between you and the clinician you saw in TIA clinic, this will not be appropriate for everyone and decisions will be made on an individual basis. If you both agree this is appropriate, it means you will not have another appointment in TIA clinic. A plan will be communicated to you and your GP by letter following your initial appointment. This will help support future management and hand over any instructions your GP will need for future action, for example when to check your cholesterol (blood test) and what we recommend your blood pressure should be. Any outstanding tests will still take place as planned and we will write with results (to you and your GP).
A follow up appointment will only be made if you request this in the next 6 months. After this time, if we have not heard from you, you will be discharged from our care.
In many specialities PIFU works well, it is safe and effective. For many people, if they feel happy they understand their diagnosis and the plan for management they do not feel further appointments are needed. This means we only see people if they feel they need to. This allows us to be more flexible and responsive when people do need to see us, meaning we can then see people quicker. We also understand if you are feeling well, you don’t want to come back to see us unnecessarily.

What are the pros and cons? Is PIFU the right pathway for me?

When to ask for help?
If you have questions about your diagnosis, your treatment (e.g. side effects of medication) or do not feel confident making or sustaining healthy lifestyle changes following your TIA and would like more support please feel free to contact us. You can ask for another appointment at any point within six months of your initial assessment if you are on a PIFU pathway.
In these situations, we would book an appointment to talk or meet with a member of the team. Please have your hospital number handy when you call (if you have this) or provide your date of birth so they can identify your hospital records.

To make another appointment please call our stroke secretarial team on:
0300 019 6406/9

What to do if you experience further TIA or Stroke symptoms

If you were to experience any future TIA symptoms you must ring 999 immediately (do not ring the team directly – 999 is the quickest and safest route). This allows you to be quickly reassessed as if any symptoms are persisting you may need acute treatment.