Spasticity and spasms
What is spasticity and spasms?
Spasticity
Spasticity is where there is an increase in muscle tone (resistance or tension in the muscle). Everyone's muscles have tone; it is how ready the muscle is to contract and what allows you to move your limbs or hold a position. Those with 'low tone' often have very heavy, floppy limbs which are not as ready to contract vs 'high tone' where the muscles are too ready to contract.
Spasticity is often described as a limb that is stiff, heavy, or difficult to move. When spasticity is severe it can be very difficult for someone else to bend a limb at all.
Spasms
Spasms are sudden, involuntary tightening or contracting of a muscle. Any muscle can be affected by spasms but the most common are the arms, legs, and trunk. If a muscle repeatedly twitches or jerks, this is known as 'clonus'. A common example of this is where your foot may repeatedly tap up and down until you apply pressure to your limb or move your foot.
Different types of spasms
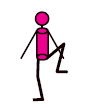
A spasm that causes a limb to bend, such as a leg moving upwards towards the body is called a flexor spasm.
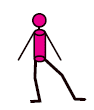
A spasm that causes a limb to extend, such as causing the leg to straighten away from the body is called an extensor spasm.
A spasm that causes a limb to be pulled in towards the body, such as making it difficult to separate thighs, is called an adductor spasm.
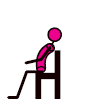
Spasms affecting the trunk can arch off a bed or away from the back of a chair.
Images from https://mstrust.org.uk/a-z/spasticity-and-spasms
What causes spasticity and spasms?
Nerve pathways that connect your brain, spinal cord and muscles, work together to coordinate smooth movement. If nerve signals between a muscle and the brain are interrupted by damage caused by MS, the muscle can remain in its shortened state. This makes the affected limb feel stiff or tight and often difficult to move. If a limb becomes fixed in this position, it is known as a contracture. Nerve messages that are interrupted can also cause overactivity of muscles and loss of coordination leading to spasms. Spasticity can happen in any part of your body, depending on which nerves in your brain or spinal cord are affected.
Symptoms that occur with spasticity and spasms
Pain
Spasticity and spasms are not always painful. If there is pain it may feel like a pulling or tugging of the muscles, particularly around joints. Sometimes spasticity and spasms can lead you to alter how you stand, sit or lie, and this can lead to pain. Movement and stretching can help manage this.
Weakness
The damaged nerve pathways can make muscles stiff or weak. This can lead to some muscles being stiff and others weak in the same limb (arm or leg). Weak limbs may feel heavy when you are trying to move them. If someone else, a loved one/ carer, can move them easily, but you are unable to, then this is likely weakness rather than spasticity. Sometimes removing all spasticity is not helpful as it leaves weakness and will make tasks harder to perform, such as walking and transferring. An assessment of your spasticity, perhaps by a physiotherapist, will identify if the stiffness in a limb is helping you to function, and whether medication to treat spasticity will be helpful or not.
What can I do to help spasticity and spasms?
It is important to keep your muscles, ligaments and joints as flexible as possible. This can be done through exercise and stretching. You may need someone to help you stretch your limbs if you are unable to move your limbs yourself. A physiotherapist will be able to advise how best to do this.
Ensuring your posture is as good as it can be is also key, whether you are standing, sitting, or lying. This may include more supportive seating, or wheelchairs, or using different cushions in bed to allow your body to positioned in a comfortable but good posture.
Sometimes medication is recommended to help with spasticity and spasms. These will normally be started at a low dose and gradually increased to where you are seeing a good response. Not all spasticity and spasms need to be treated so it is important, with the support of the MS team, to think about goals of treatment and when in your day you are most struggling with symptoms. The medication can then be tailored to keep you as strong and independent as possible. If you are having any side effects from any medication started, please contact your GP to discuss further.
Trigger factors
It is important to be aware that different symptoms can trigger spasticity and spasms to become worse. Managing these trigger factors can help reduce the effects of spasticity or spasms without the need for medication. If you are taking medication, it will not be fully effective unless any trigger factors for spasticity are also being addressed. Some examples of trigger factors are:
- An increase in body temperature (perhaps due to a fever or too much exercise)
- Infections (for example bladder or chest infections)
- If you are experiencing a relapse
- Skin irritation (including pressure sores)
- A full bladder or a catheter that is not draining correctly
- Constipation
- In-grown toenails
- Ill-fitting clothes or splints
- Pain
- Posture in chair/ bed
- Emotional stress and anxiety
Dorset Spasticity Services
At University Hospitals Dorset NHS Foundation Trust, there are two spasticity clinics run at Poole Hospital and Bournemouth Hospital. These clinics are run by a Rehabilitation Medicine Consultant and will also have a specialist neurophysiotherapist in clinics.
If your spasticity and spasms need treating, you will be advised on physical management strategies (such as stretching, both active and passive exercise) in the first instance and then may be started on medication. If this is not having the desired outcome, you may be started or switched to a different medication. If your spasticity and spasms are still not manageable, then you may be referred to the specialist spasticity service for further assessment and management.
Southampton Spasticity Service may also be accessed for those with severe spasticity and who may benefit from intrathecal treatment. More information regarding this service can be found here Intrathecal Baclofen Service :: Hampshire and Isle of Wight NHS Foundation Trust
Information adapted from https://mstrust.org.uk/a-z/spasticity-and-spasms and https://www.mssociety.org.uk/about-ms/signs-and-symptoms/spasms-and-stiffness/understanding-spasms-and-stiffness. All diagrams used can be found at https://mstrust.org.uk/a-z/spasticity-and-spasms
Sleep
Sleep plays an important role in overall health and well-being. Everyone's sleep needs are different, but for people with MS, common symptoms can often lead to disrupted or poor-quality sleep.
Importance of sleep
Restoration and Healing: during sleep the body repairs tissues, muscles, and the immune system.
Cognitive function: sleep helps memories embed, helps with problem solving, learning and creativity. It enhances your ability to focus, make decisions and process information.
Emotional regulation: a lack of sleep can cause irritability and mood swings.
Immune function: sleep strengthens the immune system allowing the body to be better equipped to fight against infections.
Stress reduction: good sleep reduces stress and the production of stress hormones which in turn supports better mental and physical health.
Hormone regulation: sleep helps to regulate hormones including ones that control appetite (leptin and ghrelin) and growth hormones. Disrupted sleep can cause imbalances which can lead to weight gain.
Sleep can be a challenge for many people with MS due to symptoms such as pain, muscle spasms and bladder issues but it can also be difficult to unpick what is due to MS and what is sometimes due to more general problems such as worry, stress, hormones and environmental factors.
General tips to sleeping well:
- Maintain a consistent sleep pattern by going to bed and waking up at the same time every day, even on weekends, to regulate your body's internal clock
- Create a relaxing bedtime routine and establish calming activities before sleep
- Consider reading, gentle stretches, breathing exercises, relaxation exercises or anything that signals time to wind down
- Make sure your sleep environment is comfortable, such as not too hot or too cold
- Limit screen time. Avoid phones, tablets, and TV at least an hour before you go to bed as the blue light can interfere with your sleep
- Be mindful of your diet. Avoid heavy or spicy meals, caffeine, and alcohol close to bedtime
- Try to get some physical movement in the day to promote better sleep but don't attempt exercises in the few hours before bedtime
- Manage your stress. Relaxation exercises, meditation, yoga, progressive muscle relaxation are all ways to try and reduce stress and anxiety
- Limit your naps. If you need to nap during the day, keep it short and no longer than 20-30 minutes at any one time, and preferably not too close to bedtime
- Watch your intake of fluids close to bedtime, especially if you have bladder issues
- Get exposure to natural light in the day, as this can regulate your sleep-wake cycle. Being outside in the daytime can help. At night, blackout blinds, or an eye mask in summer, may help with your body preparing for sleep
- If you have trouble getting to sleep, or when you wake up in the night, avoid clock-watching as this can create anxiety
- Consider a notepad beside your bed and jot down any concerns so that you can deal with worries in the morning, try to "park" your concerns
- It may take time to establish good sleep habits, so remember to be patient and consistent when trying to maintain good sleep patterns
Sleep tips specific to MS:
- Medication management: take prescribed medications for muscle spasms or other MS symptoms, especially if these interfere with your sleep. See Spasticity and Pain
- Sometimes you may need medications to get you to sleep and discussing this with your GP is important
- Manage temperature: MS can make some people very sensitive to temperature changes so keep your bedroom at a comfortable temperature to avoid overheating or getting too cold in the night. You may need to consider a different duvet or bedding to your partner
- Consider using devices, such as cooling blankets or fans, if heat sensitivity is a problem for you
- Gentle stretches can help muscle stiffness and spasms. The MS physiotherapist can advise if this is something you feel you suffer from. See Spasticity
- If you have to get up to go to the toilet frequently in the night, consider stopping drinking three hours before you go to bed. See Bladder
- Fatigue management is important in the day to prevent excessive fatigue and becoming over tired. Plan small regular rests into your day. See Fatigue
- Pain management is important for some MS symptoms, especially if they interfere with you sleeping well. If this is something you think you need to consider, discuss with your MS nurse, or contact the MS helpline for advice. See Pain
- Supportive positioning can be useful, and a good mattress can make a big difference
For further information see these links below.
https://www.nhs.uk/live-well/sleep-and-tiredness/how-to-get-to-sleep/
https://www.nhs.uk/conditions/insomnia/
https://mstrust.org.uk/information-support/wellbeing-ms/sleep
https://www.nationalmssociety.org/Living-Well-With-MS/Diet-Exercise-Healthy-Behaviors/Sleep
Relaxation
The benefits of relaxation are well known in helping to reduce fatigue levels, manage anxiety, promote better sleep, and help achieve an overall sense of well-being. MS can be unpredictable and having strategies in place to help you through relapses, or times of change/uncertainty, can be very helpful.
There are many ways that people can relax; from listening to calming music, watching the birds in the garden to using specific methods such as meditation apps or visualisation techniques.
Top tips for relaxation
- Plan relaxation into your day so it is more likely to happen
- Choose a quiet comfortable spot either lying down or sitting where you will not be disturbed
- Decide your relaxation technique, e.g. watching birds or listening to a relaxation App
- Have a blanket over you, or ensure the room is warm, as your body temperature will drop when relaxed
- Let family know not to disturb you and switch your phone to silent mode
- Set an alarm for 30 minutes in case you fall asleep. If you fall asleep for longer than 30 minutes in the day, this can interfere with your night sleep
- Practise your chosen technique – it might take a few sessions to start to feel the benefit
The MS Trust has a useful information page on relaxation with information on different relaxation techniques https://mstrust.org.uk/a-z/relaxation with an opportunity to try a relaxation session.
There are lots of Apps available to practise relaxation and mindfulness. Some of these may require ongoing payment. Here are a few examples:
https://insighttimer.com/en-gb
Information sourced from Hereford MS Wellbeing Hub (herefordmshub.co.uk)
Also see Mindfulness.
Sex and intimacy
Intimacy and sexuality can sometimes be affected by multiple sclerosis. Sexual activity and relationships can be affected by a variety of symptoms. It can be helpful to talk about sex and intimacy with your health professional, allowing you to realise you are not alone in feeling this way, and that often simple changes can make a difference.
We appreciate it may feel difficult to talk about sexual issues you may be experiencing. Please be reassured if you would like to talk, we have clinics that are private and confidential.
Below are some typical symptoms that people with MS may experience.
Women
- Loss of desire
- Vaginal dryness
- Numbness/altered sensation
- Difficulty orgasming
The most important thing is to talk about your challenges. Some people find this embarrassing, but support is there for you. We may suggest techniques to reintroduce intimacy, using lubricating gels or experimenting with sex toys such as vibrators. The MS Trust booklets for men and women outline various techniques to create a desire, such as body mapping or other games.
https://mstrust.org.uk/a-z/sexual-problems-women-ms
Men
- Loss of desire
- Erectile dysfunction
- Numbness/altered sensation
- Inability to orgasm or ejaculate
Talking about your challenges is important. The MS team are used to discussing sex with people with MS. We may suggest body mapping, gels, vibrators, or medication. We may also refer you to different services to discuss vacuum pumps, injections, or psychosexual therapy.
https://mstrust.org.uk/a-z/sexual-problems-men-ms
Talking to health professionals
Speaking with a healthcare professional about sex and intimacy issues can be beneficial and improve your self-esteem.Think about what you want to say and the words you feel comfortable using before your appointment with the MS team. Using words you are more comfortable with can help you to feel more relaxed.
Other resources
Videos:
https://www.youtube.com/watch?v=0oV-o2h1lEE
https://www.youtube.com/watch?v=bUs0v5iZEbI
Further information:
MS, sex and relationships | Shift.ms
Pain in MS
Pain
Everyone experiences pain differently – "Pain is whatever the experiencing person says it is, existing whenever they say it does". McCaffery 1969.
Pain is an uncomfortable feeling that tells you something may be wrong. It can be steady, throbbing, stabbing, aching, pinching, or described in many other ways. Sometimes, it's just a nuisance, like a mild headache. Other times it can be debilitating. It can be short or long-term and stay in one place or spread around the body.
Describing Pain
A person's description of their pain will help identify the type of pain, so we may ask you to describe:
- The character of pain, such as what does it feel like?
- The site, quality, any radiation of pain: meaning where you feel the pain and how far it seems to have spread?
- What things make the pain better or worse?
- The times when the pain occurs throughout the day?
- The effect it has on your daily abilities and mood?
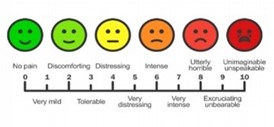
The above diagram is what we would use to measure a person's pain - VAS (Visual Analogue Scale)
Types of pain and causes in MS
- Nerve pain (neuropathic pain) - is caused by damage to the nerves in the brain and spinal cord. This includes altered sensations such as pins and needles, numbness, crawling or burning feelings. Examples of nerve pain include painful sensations in the side of the face, called trigeminal neuralgia, and a tight feeling, often around the chest, called the MS hug. Pain in the arms or legs is very common.
- Musculoskeletal pain - is caused by damage to muscles, tendons, ligaments and soft tissue, for example: neck or back pain caused by changes in posture or sitting for very long periods, or injury.
How to manage pain
Pain is a very common symptom in MS.
Pain signals use the spinal cord and specialised nerve fibres to travel to your brain. Part of this process is linked directly with the emotional centres in the brain. This means how you are feeling influences your pain. If you feel angry, depressed or anxious, your pain will be worse.
The opposite is also true. If you are feeling positive and happy, your pain can seem less, and you are able to cope better.
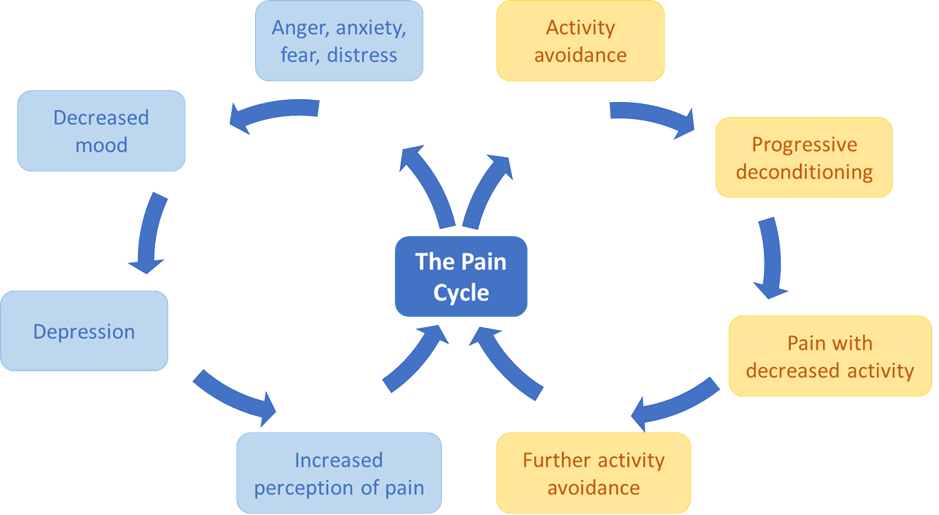
Pain is never "just in the mind" or "just in the body" - it is a complex mix and how the brain interprets the signals. This mix can change from one day to the next.
Managing pain
Medication
Nerve pain
Common painkillers are not usually effective against nerve pain, therefore NICE (National Institute for Health and Care Excellence) recommends that people with MS should try amitriptyline, gabapentin, pregabalin, or duloxetine, first. Your neurologist or GP will need to prescribe these medications. Treatment usually starts with a low dose and then builds up slowly until an effective dose is reached. These medications are unlikely to provide complete pain relief but should reduce the pain intensity (a bit like a dimmer switch for a light).
Musculoskeletal pain
Musculoskeletal pain may be helped by common pain-relieving drugs such as paracetamol, ibuprofen or aspirin. https://www.mskdorset.nhs.uk/ is a good source of information about how to manage common musculoskeletal problems.
If the pain is due to muscle stiffness (spasticity), then treatments for spasticity may be offered.
Other ways to manage pain
Exercise
Lack of activity and exercise, due to pain or other symptoms, can cause a gradual loss of strength and fitness. This is called deconditioning and can make your pain worse. Although it may not sound appealing if you are in pain, regular exercise can reverse deconditioning and help ease your pain. Link to exercise and activity.
Posture
Poor posture can develop gradually particularly if you have MS. Simple changes to improve posture when sitting, standing or lying down can help relieve stress on the muscles, joints and ligaments which may help reduce aches and pains. Posture and MS | MS Trust.
Heat
Although heat sensitivity makes MS symptoms worse for many people, heat applied to the affected area can be helpful.
Cold
Some people find that applying ice or a cold pack helps. Ice should be wrapped in a tea towel not applied straight to the skin or you could try a pack of frozen peas.
Relaxation
There are many relaxation techniques which can help you so it can be worth trying a range to see what suits you best. You could try breathing exercises, massage, mindfulness, meditation, hypnotherapy or gentle yoga stretching exercises. See Mindfulness and Relaxation for more information.
TENS
Transcutaneous electrical nerve stimulation is the application of a small electric current. It can be used in the management of some types of pain in MS.
Dorset Pain Management service
If your pain is particularly problematic, and other ways of managing it have been unsuccessful, your GP or MS Service may consider referring you to the Dorset Pain Management Service.
This service supports people to develop new skills to understand their body and deal with pain with greater knowledge and confidence. This helps people come to terms with their pain and adopt effective strategies for living life meaningfully.
https://dorsetpain.org.uk/#Opt-In
Other Useful Links:
https://www.mssociety.org.uk/about-ms/signs-and-symptoms/pain
https://mstrust.org.uk/a-z/pain#types-of-pain
Information sourced from Hereford MS Wellbeing Hub (herefordmshub.co.uk)









