Pain in MS
Pain
Everyone experiences pain differently – "Pain is whatever the experiencing person says it is, existing whenever they say it does". McCaffery 1969.
Pain is an uncomfortable feeling that tells you something may be wrong. It can be steady, throbbing, stabbing, aching, pinching, or described in many other ways. Sometimes, it's just a nuisance, like a mild headache. Other times it can be debilitating. It can be short or long-term and stay in one place or spread around the body.
Describing Pain
A person's description of their pain will help identify the type of pain, so we may ask you to describe:
- The character of pain, such as what does it feel like?
- The site, quality, any radiation of pain: meaning where you feel the pain and how far it seems to have spread?
- What things make the pain better or worse?
- The times when the pain occurs throughout the day?
- The effect it has on your daily abilities and mood?
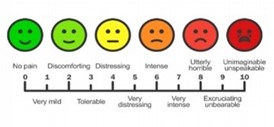
The above diagram is what we would use to measure a person's pain - VAS (Visual Analogue Scale)
Types of pain and causes in MS
- Nerve pain (neuropathic pain) - is caused by damage to the nerves in the brain and spinal cord. This includes altered sensations such as pins and needles, numbness, crawling or burning feelings. Examples of nerve pain include painful sensations in the side of the face, called trigeminal neuralgia, and a tight feeling, often around the chest, called the MS hug. Pain in the arms or legs is very common.
- Musculoskeletal pain - is caused by damage to muscles, tendons, ligaments and soft tissue, for example: neck or back pain caused by changes in posture or sitting for very long periods, or injury.
How to manage pain
Pain is a very common symptom in MS.
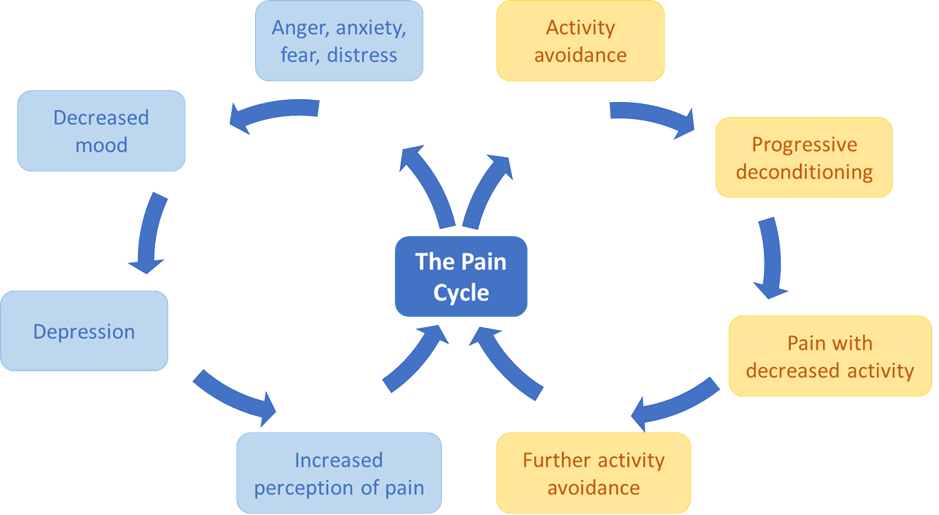
Pain signals use the spinal cord and specialised nerve fibres to travel to your brain. Part of this process is linked directly with the emotional centres in the brain. This means how you are feeling influences your pain. If you feel angry, depressed or anxious, your pain will be worse.
The opposite is also true. If you are feeling positive and happy, your pain can seem less, and you are able to cope better.
Pain is never "just in the mind" or "just in the body" - it is a complex mix and how the brain interprets the signals. This mix can change from one day to the next.
Managing pain
Medication
Nerve pain
Common painkillers are not usually effective against nerve pain, therefore NICE (National Institute for Health and Care Excellence) recommends that people with MS should try amitriptyline, gabapentin, pregabalin, or duloxetine, first. Your neurologist or GP will need to prescribe these medications. Treatment usually starts with a low dose and then builds up slowly until an effective dose is reached. These medications are unlikely to provide complete pain relief but should reduce the pain intensity (a bit like a dimmer switch for a light).
Musculoskeletal pain
Musculoskeletal pain may be helped by common pain-relieving drugs such as paracetamol, ibuprofen or aspirin. https://www.mskdorset.nhs.uk/ is a good source of information about how to manage common musculoskeletal problems.
If the pain is due to muscle stiffness (spasticity), then treatments for spasticity may be offered.
Other ways to manage pain
Exercise
Lack of activity and exercise, due to pain or other symptoms, can cause a gradual loss of strength and fitness. This is called deconditioning and can make your pain worse. Although it may not sound appealing if you are in pain, regular exercise can reverse deconditioning and help ease your pain. Link to exercise and activity.
Posture
Poor posture can develop gradually particularly if you have MS. Simple changes to improve posture when sitting, standing or lying down can help relieve stress on the muscles, joints and ligaments which may help reduce aches and pains. Posture and MS | MS Trust.
Heat
Although heat sensitivity makes MS symptoms worse for many people, heat applied to the affected area can be helpful.
Cold
Some people find that applying ice or a cold pack helps. Ice should be wrapped in a tea towel not applied straight to the skin or you could try a pack of frozen peas.
Relaxation
There are many relaxation techniques which can help you so it can be worth trying a range to see what suits you best. You could try breathing exercises, massage, mindfulness, meditation, hypnotherapy or gentle yoga stretching exercises. See Mindfulness and Relaxation for more information.
TENS
Transcutaneous electrical nerve stimulation is the application of a small electric current. It can be used in the management of some types of pain in MS.
Dorset Pain Management service
If your pain is particularly problematic, and other ways of managing it have been unsuccessful, your GP or MS Service may consider referring you to the Dorset Pain Management Service.
This service supports people to develop new skills to understand their body and deal with pain with greater knowledge and confidence. This helps people come to terms with their pain and adopt effective strategies for living life meaningfully.
https://dorsetpain.org.uk/#Opt-In
Other Useful Links:
https://www.mssociety.org.uk/about-ms/signs-and-symptoms/pain
https://mstrust.org.uk/a-z/pain#types-of-pain
Information sourced from Hereford MS Wellbeing Hub (herefordmshub.co.uk)









