Spasticity and spasms
What is spasticity and spasms?
Spasticity
Spasticity is where there is an increase in muscle tone (resistance or tension in the muscle). Everyone's muscles have tone; it is how ready the muscle is to contract and what allows you to move your limbs or hold a position. Those with 'low tone' often have very heavy, floppy limbs which are not as ready to contract vs 'high tone' where the muscles are too ready to contract.
Spasticity is often described as a limb that is stiff, heavy, or difficult to move. When spasticity is severe it can be very difficult for someone else to bend a limb at all.
Spasms
Spasms are sudden, involuntary tightening or contracting of a muscle. Any muscle can be affected by spasms but the most common are the arms, legs, and trunk. If a muscle repeatedly twitches or jerks, this is known as 'clonus'. A common example of this is where your foot may repeatedly tap up and down until you apply pressure to your limb or move your foot.
Different types of spasms
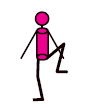
A spasm that causes a limb to bend, such as a leg moving upwards towards the body is called a flexor spasm.
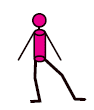
A spasm that causes a limb to extend, such as causing the leg to straighten away from the body is called an extensor spasm.
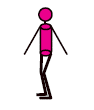
A spasm that causes a limb to be pulled in towards the body, such as making it difficult to separate thighs, is called an adductor spasm.
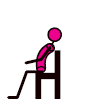
Spasms affecting the trunk can arch off a bed or away from the back of a chair.
Images from https://mstrust.org.uk/a-z/spasticity-and-spasms
What causes spasticity and spasms?
Nerve pathways that connect your brain, spinal cord and muscles, work together to coordinate smooth movement. If nerve signals between a muscle and the brain are interrupted by damage caused by MS, the muscle can remain in its shortened state. This makes the affected limb feel stiff or tight and often difficult to move. If a limb becomes fixed in this position, it is known as a contracture. Nerve messages that are interrupted can also cause overactivity of muscles and loss of coordination leading to spasms. Spasticity can happen in any part of your body, depending on which nerves in your brain or spinal cord are affected.
Symptoms that occur with spasticity and spasms
Pain
Spasticity and spasms are not always painful. If there is pain it may feel like a pulling or tugging of the muscles, particularly around joints. Sometimes spasticity and spasms can lead you to alter how you stand, sit or lie, and this can lead to pain. Movement and stretching can help manage this.
Weakness
The damaged nerve pathways can make muscles stiff or weak. This can lead to some muscles being stiff and others weak in the same limb (arm or leg). Weak limbs may feel heavy when you are trying to move them. If someone else, a loved one/ carer, can move them easily, but you are unable to, then this is likely weakness rather than spasticity. Sometimes removing all spasticity is not helpful as it leaves weakness and will make tasks harder to perform, such as walking and transferring. An assessment of your spasticity, perhaps by a physiotherapist, will identify if the stiffness in a limb is helping you to function, and whether medication to treat spasticity will be helpful or not.
What can I do to help spasticity and spasms?
It is important to keep your muscles, ligaments and joints as flexible as possible. This can be done through exercise and stretching. You may need someone to help you stretch your limbs if you are unable to move your limbs yourself. A physiotherapist will be able to advise how best to do this.
Ensuring your posture is as good as it can be is also key, whether you are standing, sitting, or lying. This may include more supportive seating, or wheelchairs, or using different cushions in bed to allow your body to positioned in a comfortable but good posture.
Sometimes medication is recommended to help with spasticity and spasms. These will normally be started at a low dose and gradually increased to where you are seeing a good response. Not all spasticity and spasms need to be treated so it is important, with the support of the MS team, to think about goals of treatment and when in your day you are most struggling with symptoms. The medication can then be tailored to keep you as strong and independent as possible. If you are having any side effects from any medication started, please contact your GP to discuss further.
Trigger factors
It is important to be aware that different symptoms can trigger spasticity and spasms to become worse. Managing these trigger factors can help reduce the effects of spasticity or spasms without the need for medication. If you are taking medication, it will not be fully effective unless any trigger factors for spasticity are also being addressed. Some examples of trigger factors are:
- An increase in body temperature (perhaps due to a fever or too much exercise)
- Infections (for example bladder or chest infections)
- If you are experiencing a relapse
- Skin irritation (including pressure sores)
- A full bladder or a catheter that is not draining correctly
- Constipation
- In-grown toenails
- Ill-fitting clothes or splints
- Pain
- Posture in chair/ bed
- Emotional stress and anxiety
Dorset Spasticity Services
At University Hospitals Dorset NHS Foundation Trust, there are two spasticity clinics run at Poole Hospital and Bournemouth Hospital. These clinics are run by a Rehabilitation Medicine Consultant and will also have a specialist neurophysiotherapist in clinics.
If your spasticity and spasms need treating, you will be advised on physical management strategies (such as stretching, both active and passive exercise) in the first instance and then may be started on medication. If this is not having the desired outcome, you may be started or switched to a different medication. If your spasticity and spasms are still not manageable, then you may be referred to the specialist spasticity service for further assessment and management.
Southampton Spasticity Service may also be accessed for those with severe spasticity and who may benefit from intrathecal treatment. More information regarding this service can be found here Intrathecal Baclofen Service :: Hampshire and Isle of Wight NHS Foundation Trust
Information adapted from https://mstrust.org.uk/a-z/spasticity-and-spasms and https://www.mssociety.org.uk/about-ms/signs-and-symptoms/spasms-and-stiffness/understanding-spasms-and-stiffness. All diagrams used can be found at https://mstrust.org.uk/a-z/spasticity-and-spasms









